Tophaceous Gout Causing Atlanto-Axial Subluxation
An 82-year-old man with hypertension and gout developed periods of dizziness, neck pain, and arm weakness. Could the gout be responsible?
An 82-year-old African American male with a history of hypertension and polyarticular tophaceous gout presented to the emergency department (ED) with acute onset of dizziness, neck pain, and bilateral upper extremity weakness that had arisen periodically over the previous two months.
He described his neck pain as 10 o n a scale of 1 to 10, aching, non-radiating, associated with movement and worst in the morning. He attributed the pain to his sleeping posture. His symptoms had progressed in the two weeks prior to admission, culminating in numbness and weakness in the hands. He reported two episodes of syncope while turning his head, one at the dentist’s office and another during a car ride. On both occasions syncopal episode was preceded by dizziness, tingling, and numbness in his arms and accompanied by weakness, nausea, and visual disturbances. He denied postictal confusion, urine or stool incontinence, or any history of trauma.
His home medications included 0.6 mg colchicine and 100 mg allopurinol, both daily, for crystal-proven gout that was diagnosed 30 years ago. His most recent gout flare was 2 years ago. He reported that each flare lasts for 10 days, with joint pain and swelling.
On physical examination, the patient appeared in moderate distress due to neck pain as he was lying in bed. Vital signs on arrival to the ED were unremarkable for his advanced age. He was oriented to time, place and person.
Noteworthy laboratory findings on admission were sedimentation rate (10 mm/hr), CRP (<2.9mg/l) and uric acid level (4.9 mg/dl). RF and CCP antibody levels were within normal ranges.
The musculoskeletal exam showed:
• C-Spine: upper cervical and paracervical tenderness. Severe limitations of passive and active flexion (<45°), rotation (<70°), lateral bending (<40°), and extension (<45°). Full range of movement of temporomandibular joint with no tenderness or crepitus.
• Hands: Heberden’s and Bouchard’s nodes in the PIP and DIP bilaterally. Multiple subcutaneous nodules over the MCP, PIP, and DIP bilaterally. No discrete synovitis was noted.
• Elbows: Multiple subcutaneous nodules with synovial thickening of the olecranon bursa bilaterally.
• Shoulders: Deltoid muscle atrophy. Limitation of flexion and extension (<90°), external rotation and internal rotation (40°), adduction (20°), and abduction (<90°).
• Neurological Exam: Cranial nerves II-XII intact. Sensation to touch and pinprick wasintact. Power was 3/5 in the upper extremity proximal and distal muscles and 5/5 wasthe lower extremity. Reflexes were decreased bilaterally in the upper extremity and normal in the lower extremity. Normal gait.
The rest of the physical exam did not reveal any abnormality.
For the imaging findings, see the next page.

Radiographs of the upper extremities revealed numerous tophi in elbows, wrists, and hands (left.)
Erosions with overhanging edges were present in the distal ulnar, carpal bones, and first, second, and fifth metacarpals. (below, right) Carpal bones in both hands showed extensive avulsions with partial fusion.
Extensive erosive changes with overhanging margins were visible in the proximal and distal interphalangeal and metacarpophalangeal joints. Soft tissue swelling was present around both wrist joints.

Cervical spine X-rays (below) showed diffuse osteopenia with maintained vertebral body heights. However, the area of the superior bands was not well delineated. There was no evidence of acute fracture or subluxation in neutral, flexion or extension views. Extensive spurring was visible at the C1-C2 articulation, with large anterior spurs present from C2 to C4 and complete or near complete bridging anteriorly. Narrowing of the disc space was observed at C2/C3, C4/C5, C5/C6 and C6/C7. There was partial fusion of C5 and C6 vertebral bodies and straightening of normal cervical lordosis.

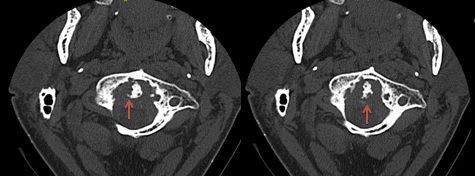
A CT scan of the cervical spine showed destruction and separation of the dens, with erosive changes (red arrows, below).
Soft tissue attenuation around the C1-dens articulation with faint calcifications was suggestive of pannus (red arrow, right) that was causing effacement of the thecal sac and mild cervical spinal cord displacement posteriorly.
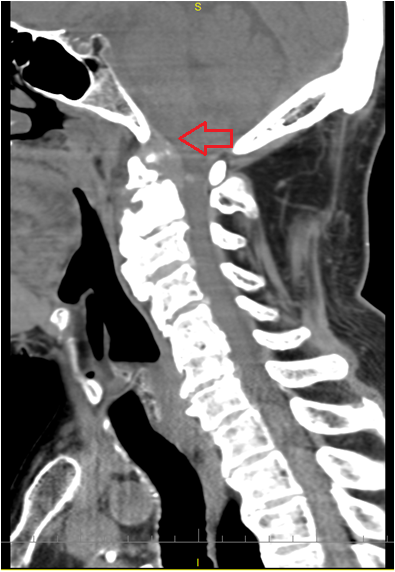
There was straightening of the cervical spine with moderate-to-severe degenerative changes (anterior osteophytosis as well as marginal osteophytosis at all cervical vertebral levels). The intervertebral disc spaces of C2-C3, C4-C5, C5-C6 and C6-C7 were decreased, with subtle erosive changes along the endplates. The C5-C6 vertebral bodies were partially fused.
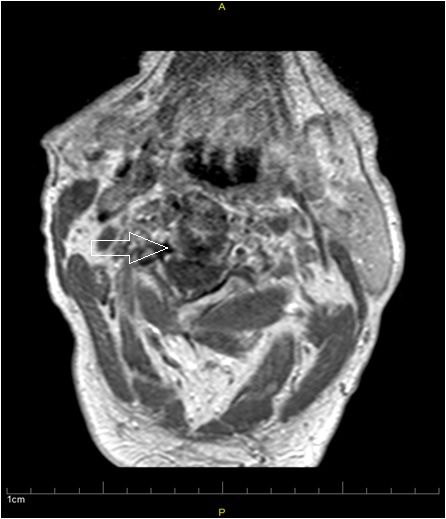
MRI of the cervical spine (below) revealed erosive arthritis with callous formation involving the C1-C2 joint and odontoid process. There was mild narrowing of the foramen magnum and proximal cervical spinal canal, with a slight alteration of the course of the proximal cervical spinal cord but no evidence of cord compression or myelomalacia.
Destructive and erosive changes were visible in the odontoid process, associated with enhancement of soft tissue consistent with pannus (arrow, below right).

Given our patient’s long history of polyarticular tophaceous gout, supported by the findings from imaging, we attributed his neck pain and upper extremity weakness to erosion of the cervical spine caused by his gout.
These kinds of lesions can occur in any area of the cervical spine, but are most frequently seen at the level of C4-C7.1,2 We found his presentation with erosion at the upper level of the cervical spine unusual and therefore interesting.
For the Discussion and Outcome, see the next page.
DISCUSSION:
When we initially evaluated the patient, the differential was:
1. Crystal arthropathy: Gout and /or Pseudogout (Calcium Pyrophosphate Deposition)
2. Rheumatoid Arthritis
3. TB
4. Malignancy
5. Syphilis
The patient had a history of crystal-proven gout diagnosed 30 years ago. Our review of his electronic medical records over a period of 14 years revealed 14 uric acid measurements ranging between 4.9 and 9.9, with 11 of them being >7.0. Arthrocentesis reported in 2004 revealed only monosodium urate (MSU) crystals, and again in 2013 when the patient was under our care, we identified MSU crystals, both intracellular and extracellular, on polarized light microscopic evaluation of synovial fluid.
The differential diagnosis for crystal arthopathies includes calcium pyrophosphate deposition (CPPD), hydroxyapatite disease, and gout. CPPD is a common finding in this patient’s age group, and can be seen incidentally without any symptoms. However, multiple previous radiographs of the wrist and knee, the most common sites for manifestations of CPPD, showed no findings of chondrocalcinosis
While tophi can become calcified, the prominence of calcifications could reflect coexistent chondrocalcinosis. Although radiographs of the shoulder and knee joints did not reveal chondrocalcinosis, those of the wrist did show chondrocalcinosis. However, no calcium pyrophosphate crystals were observed. Although coexistent gout and pseudogout is a possibility, in the absence of calcium pyrophosphate crystals were were unable to make a definitive diagnosis.
Another possibility is hydroxappatite deposition, which can be indistinguishable from CPPD and can cause “crowned dens syndrome.”3 Its typical manifestations include:
1. calcific deposits of annulus fibrous and transverse ligament of the dens
2. calcific deposits of supraspinous and infraspinous ligaments and intervertebral discs
3. capsular calcification in the apophyseal facet joints
4. periodontoid mass of the foramen magnum
We do not feel that the erosive changes and faint calcifications we observed are consistent with a diagnosis of hydroxyapatite deposition.
After discussion of the differential with radiology, we concluded that the long history of gout, added to the CT and MRI findings, favored a diagnosis of tophaceous deposition. Bone erosions near the urate crystal deposits and secondary proliferative bone changes, in addition to CT findings of low-density areas representing tophi, are features of spinal gout.
OUTCOME:
We recommended that the patient continue colchicine and allopurinol and consider adding uricase. He was also evaluated by neurosurgery; no intervention was recommended and he was given a cervical collar.
A recent carotid Doppler and magnetic resonance angiogram showed that the right vertebral artery appeared to have antegrade flow with a lack of diastolic flow, consistent with a distal occlusion. He was diagnosed with right cerebellar artery occlusion, and commenced treatment with acetylsalicylic acid and statins.
REFERENCES
1. Kersley GD, Mandel L, Jeffrey MR. Gout: an usual case with softening and subluxation of the first cervical vertebra and splenomegaly.Ann Rheum Dis (1950) 9:282-304.
2. Thavarajah D, Hussain R, Martin JL. (2010) Cervical arthropathy caused by gout: stabilization without decompression.Eur Spine J 20 (Suppl 2): S231-S234
3. Uh M, Dewar C, Spouge D Blocka K. Crowned dens syndrome: a rare cause of acute neck pain.Clin Rheumatol. (2013) 32:711-714