Imaging for Elastofibroma Dorsi Diagnosis
Accurate diagnosis of elastofibroma dorsi may be achieved with a proper clinical history, knowledge of the characteristic site of the lesion, and typical imaging findings to avoid unnecessary biopsy and surgery.
ABSTRACT: Accurate diagnosis of elastofibroma dorsi may be achieved with a proper clinical history, knowledge of the characteristic site of the lesion, and typical imaging findings to avoid unnecessary biopsy and surgery. The lesion may easily be misinterpreted as a neoplasm, but it has characteristic imaging features in ultrasonography, CT, and MRI. To better understand the imaging features, physicians should know about the pathological characteristics. The gross histology of elastofibroma typically involves a multilayered background of elastofibrous tissue alternating with fatty streaks, which provides the typical imaging features in the various modalities. Because MRI has high resolution and the findings are the most closely correlated with the pathology, it is considered to be the modality of choice. (J Musculoskel Med. 2011;28:254-256)
Elastofibroma dorsi is a rare pseudotumor that develops in a highly characteristic anatomical location. With a proper clinical history, knowledge of the characteristic site of the lesion, and typical imaging findings, accurate diagnosis may be achieved to avoid unnecessary biopsy and surgery.
Radiologists who are unfamiliar with the features of elastofibroma dorsi may easily misinterpret it as a neoplasm. However, the lesion shows characteristic imaging features in ultrasonography (US), CT, and MRI, which in most cases may allow for a definitive diagnosis. In this case report, we emphasize the importance of gaining a better understanding of the features of elastofibroma with various imaging modalities, particularly US, to make the appropriate diagnosis.
Case report
A 78-year-old woman presented with an asymptomatic left subscapular mass that had been present for 2 years. The mass was nontender and static in size. Physical examination showed a 5-cm firm subcutaneous mass over the left subscapular region. The provisional clinical diagnosis was lipoma.
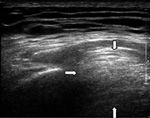
Figure 1 –
In the patient in our case report, the presenting mass was a predominantly hyperechoic lesion with a rather ill-defined border (arrows) as seen on ultrasonography. The posterior border was not well delineated, which is suggestive of high cellularity and acoustic shadowing. Internal hypoechoic streakiness was present within the lesion. There was no calcification or cystic component.
US showed a mass between the rhomboid major muscles and chest wall (Figure 1). The differential diagnosis included lipoma and fibrous tumor. CT was performed subsequently for further evaluation; it showed an elliptical soft tissue mass with intralesional streaks of fat in the left subscapular region (Figure 2). Within the soft tissue lesion, the hypoechoic component represented fibrous tissue and the hyperechoic component represented fat.
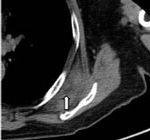
Figure 2 –
A CT scan shows a lesion isodense to the adjacent skeletal muscle (arrow). There were streaks of fat density within the lesion, which showed no infiltration to the adjacent fat and structure. The adjacent scapula was not eroded. There was no calcification or cystic component.
The imaging features together with the characteristic sites of the lesion were consistent with elastofibroma dorsi. One year later, follow-up MRI showed no growth and confirmed the presence of fibrous tissue interposed with lipomatous tissue that is characteristic of elastofibroma dorsi (Figure 3).
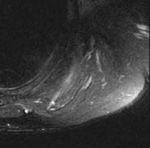
Figure 3 –
A T2-weighted MRI scan shows a predominance of T2 hypointense signal, which suggests a fibrous type of tumor.
Discussion
Elastofibroma dorsi is a benign, slow-growing reactive pseudotumor of connective tissue; the lesion is elliptical, with the longer axis in the craniocaudal direction over the subscapular and infrascapsular regions. Elastofibroma dorsi is characterized by fibroblastic proliferation and accumulation of abnormal elastic fiber alternating with deposition of hyperplastic fat,1,2 possibly the result of repeated microtrauma between the scapula and chest wall during heavy physical labor.3
The lesion characteristically is located in the lower periscapular region, usually subscapular and infrascapular, between the scapula and chest wall deep to the serratus anterior, latissimus dorsi, and rhomboid major muscles, and typically extends from the sixth to the eighth ribs.1,3 Atypical sites include the extremities, ischial tuberosities, small intestine, colon, intraspinal space, and tracheobronchial trees and within the thoracic wall.2-4
In some of the case series, 10% to 66% of lesions are bilateral.5,6 Bilateralism further supports the diagnosis of elastofibroma,7 as demonstrated in this case. The bilateralism may be symmetrical or asymmetrical. If the diagnosis of elastofibroma is suspected clinically, imaging of both sides of the chest wall for comparison is important.
The incidence of elastofibroma dorsi at autopsy is up to 24% in women and 11% in men.3 However, clinical presentation of the disease is rare. Elastofibroma usually occurs in older persons (mean age, 70 years)2,5; few cases have been documented in persons younger than 50 years.6 More than 50% of cases are asymptomatic.1,3,5 The main symptoms are an enlarging soft tissue mass; shoulder pain and discomfort; and “locking,” or “snapping.”1
To better understand the imaging features of elastofibroma, physicians should know about the pathological characteristics. The gross histology of elastofibroma typically involves a multilayered background of elastofibrous tissue alternating with fatty streaks, which provides the typical imaging features in the various modalities.
US, which occasionally is performed before other imaging studies, reveals a peculiar echotexture composed of arrays of interspersed linear or curvilinear hypoechoic strands on an echogenic background that are roughly parallel to the chest wall. Hypoechoic strands are compatible with areas of fat, and the echogenic background reflects the predominantly fibroelastic bulk of the mass.5 There is no significant flow in color Doppler sonograms.5
US has an advantage over cross-sectional imaging (CT or MRI) in that it allows for dynamic scanning-the mass is more conspicuous with scanning of patients prone with their arms abducted.6 Although the differential diagnosis includes lipoma and lipomatous tumor, the US features of a fibrous lesion with interposed fatty strands are more suggestive of elastofibroma dorsi. Recognition of these findings, which usually are overlooked, can avoid unnecessary biopsy.
The reported prevalence of this tumor was 2% in a study of patients older than 60 years who were undergoing chest CT for evaluation of pulmonary parenchyma.4 CT usually features an infrascapular or subscapular poorly defined soft tissue mass, with attenuation similar to that of adjacent skeletal muscles, containing internal striation or scattered areas of fat attenuation.4 CT usually shows the absence of bone abnormalities.2
Because MRI has high resolution and the findings are the most closely correlated with the pathology, it is considered to be the modality of choice. A predominance of hypointense lesions is seen on all pulse sequences, with signal intensity similar to that of the adjacent skeletal muscles corresponding to the fibroelastic tissue. Streaks of fat are seen as a high-intensity signal on T1-weighted images and as an intermediate signal on T2-weighted images (see Figure 3).
There is variable signal intensity in some cases, with a predominance of low signal (decreased cellularity and abundant collagen formation) or of high signal (large amounts of intralesional fat).2,3 MRI usually shows heterogeneous contrast enhancement, probably because of the progressive accumulation of contrast in fibrous tissue.3 In 2 case reports, elastofibroma demonstrated low- to moderate-grade diffuse 18F-fluorodeoxyglucose uptake,1,8 which suggested its hypermetabolism.
The major differential diagnoses of the lesion at the subscapular site include metastases and soft tissue sarcoma (such as liposarcoma), which are easily differentiated from elastofibroma by their lack of a well-defined multilayered pattern.5 Other lesions included in the differential, such as a fibrous or fat-containing tumor, also can be separated from elastofibroma dorsi.3
Fibrous lesions appear hypointense on T2-weighted sequences and generally without the hyperintense fatty septations on T1-weighted images because of their poor cellularity and predominantly fibrous tissue; these lesions include desmoid tumor, neurofibroma, fibroma, and malignant fibrous histocytoma.3 However, lipoma, liposarcoma, and hemangioma appear hyperintense on T1-weighted images and do not show the typical T1- and T2-weighted streaked pattern of fatty septations.
Surgery is reserved for patients with symptoms; recurrence is rare.2,4 For asymptomatic patients, follow-up is advocated and biopsy is considered unnecessary if the imaging findings show the typical features.9 No cases of malignant transformation have been reported.3,6
Conclusion
With knowledge of the typical location of the tumor, the age and sex of the patient, and the characteristic radiological findings, the diagnosis of elastofibroma dorsi may be made initially with US without a need for biopsy or surgery. CT may be used to confirm the diagnosis, and if there is a suspected or inconsistent feature seen on US or CT, MRI is useful for better characterizing the lesion.
References:
References
1. Pierce JC 3rd, Henderson R. Hypermetabolism of elastofibroma dorsi on PET-CT. AJR. 2004;183:35-37.
2. Muratori F, Esposito M, Rosa F, et al. Elastofibroma dorsi: 8 case reports and a literature review. J Orthop Traumatol. 2008;9:33-37.
3. Faccioli N, Foti G, Comai A, et al. MR imaging findings of elastofibroma dorsi in correlation with pathological features: our experience. Radiol Med. 2009;114:1283-1291.
4. Ochsner JE, Sewall SA, Brooks GN, Agni R. Best cases from the AFIP: elastofibroma dorsi. Radiographics. 2006;26:1873-1876.
5. Bianchi S, Martinoli C, Abdelwahab IF, et al. Elastofibroma dorsi: sonographic findings. AJR. 1997;169:1113-1115.
6. Dalal A, Miller TT, Kenan S. Sonographic detection of elastofibroma dorsi. J Clin Ultrasound. 2003;31:375-378.
7. Naylor MF, Nascimento AG, Sherrick AD, McLeod RA. Elastofibroma dorsi: radiologic findings in 12 patients. AJR. 1996;167:683-687.
8. Patrikeos A, Breidahl W, Robins P. F-18 FDG uptake associated with Elastofibroma dorsi. Clin Nucl Med. 2005;30:617-618.
9. Domanski HA, Carlén B, Sloth M, Rydholm A. Elastofibroma dorsi has distinct cytomorphologic features, making diagnostic surgical biopsy unnecessary: cytomorphologic study with clinical, radiologic, and electron microscopic correlations. Diagn Cytopathol. 2003;29:327-333.