Woody Skin and Eosinophilia in a Young Man
A 27-year-old white man, an active-duty soldier who previously had been healthy, presented with a 5-month history of progressively worsening swelling, pain and, eventually, skin hardening in both legs and then arms
A 27-year-old white man, an active-duty soldier who previously had been healthy, presented with a 5-month history of progressively worsening swelling, pain and, eventually, skin hardening in both legs and then arms. Associated symptoms included myalgia, fever, and fatigue. There was no clear toxin exposure or change in diet or medications. The patient, who was very physically active, engaged in strenuous daily activities.
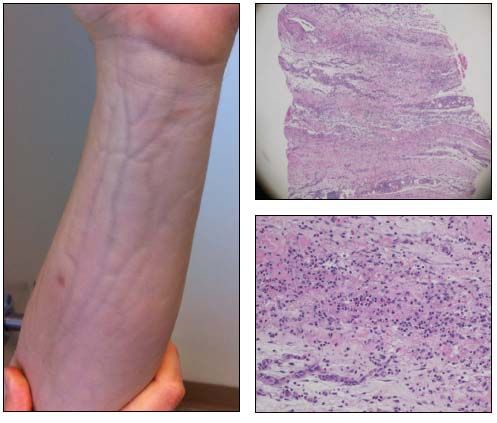
On presentation, the patient was afebrile. The physical examination was notable for mild wrist contractures without synovitis. Taut and woody indurated skin was seen on the bilateral upper and lower extremities but spared the fingers, chest, feet, back, face, and neck. This classic finding is shown in the photograph (left). What term is used to describe it?
Laboratory studies were remarkable for peripheral eosinophilia (eosinophils up to 28%), mild elevation of inflammatory markers, and an elevated IgG level but a normal IgE level. Pertinent findings were negative or normal: serum protein electrophoresis test; HIV test; and antinuclear antibodies, creatine kinase, thyroid-stimulating hormone, and serum glucose levels. A full-thickness biopsy specimen of the patient's forearm (pathology slides, below) revealed panniculitis and underlying fasciitis, with lymphocytes, plasma cells, and eosinophils.
The clinical, laboratory, and pathological findings make this a classic presentation of what disease?(Click here for the answer and discussion.)
The diagnosis was eosinophilic fasciitis (EF), also known as Shulman disease. The photograph of the patient’s elevated left forearm depicts a groove sign, defined as taut, woody skin induration with longitudinal depressions overlying the course of blood vessels.1 This classic finding is frequently seen in patients with EF,2 in which the skin induration affects the extremities but spares the fingers and toes. Peripheral eosinophilia and hypergammaglobulinemia are common laboratory findings. Panniculitis with underlying fasciitis confirms the diagnosis.
EF, or diffuse fasciitis with eosinophilia, was first described by Shulman3 in 1974. EF is a rare connective-tissue disease, with features distinct from those of systemic sclerosis (SSc). Skin induration is not only common in EF, a scleroderma variant, but is also the hallmark of SSc and a reason why the conditions often are confused.1 Distinguishing between EF and SSc is important because the treatment and prognosis differ.
SSc often involves internal organs and is associated with cutaneous telangiectasia or Raynaud phenomenon; EF rarely has those features. The distribution of skin induration is markedly different, often being widespread and symmetrical in SSc.1 Skin induration in patients with EF often has symmetrical limb involvement, sparing the trunk.
Patients with EF typically present with myalgia and arthralgia. Complications may include compartment syndrome, myopathy, carpal tunnel syndrome, inflammatory arthritis, contractures, and peripheral neuropathies. EF has a better prognosis than SSc, which has a lifelong, chronic course. EF has rare associations with myelodysplastic, lymphoproliferative, and hematological disorders.4
The diagnosis of EF is based on the patient’s clinical presentation, but a full-thickness skin biopsy and careful histopathological evaluation usually are mandated. As in the case described here, full-thickness biopsy specimens typically reveal panniculitis and underlying fasciitis, with lymphocytes, plasma cells, and eosinophils.
In addition to the typical histopathological findings, the clinical presentation helps differentiate EF from mimickers. Scleroderma variant conditions, unrelated to but often confused with SSc, are a heterogeneous group that includes EF, diffuse morphea, scleromyxedema, scleredema, eosinophilia-myalgia syndrome, and nephrogenic fibrosing syndrome.1
Although the causes of scleroderma variant conditions remain unknown, they have been associated with metabolic abnormalities and environmental, drug, and dietary exposures. EF has been linked to l-tryptophan use, toxic oil exposure, an increase in strenuous activity or exercise, and fire ants, as well as other factors.5-7
Treatment of patients with EF is centered on high-dose corticosteroids. An early start of such therapy at the onset of first symptoms provides better results than a delay in treatment.8 For patients with corticosteroid-refractory disease, other therapeutic options have been found to be effective, including cyclosporine, hydroxychloroquine, methotrexate, and tumor necrosis factor α inhibitors.9 Our patient’s symptoms improved after a few months of therapy with high-dose corticosteroids.
This case demonstrates a classic presentation of a rare connective-tissue disease. For patients with skin induration, myalgia, arthralgia, and peripheral eosinophilia, the diagnosis of EF must be entertained and full-thickness biopsy is crucial for excluding alternative diagnoses.
References:
REFERENCES
1. Varga J, Paller AS. Localized forms of scleroderma, scleroderma-like syndromes and cutaneous fibroses. Rheumatology e-dition. 4th ed. Philadelphia: Elsevier; 2008:chap 136.
2. Servy A, Clérici T, Malines C, et al. Eosinophilic fasciitis: a rare skin sclerosis. Patholog Res Int. 2010;2011:716935.
3. Shulman LE. Diffuse fasciitis with eosinophilia: a new syndrome? Trans Assoc Am Physicians. 1975;88:70-86.
4. Khanna D, Verity A, Grossman JM. Eosinophilic fasciitis with multiple myeloma: a new haematological association. Ann Rheum Dis. 2002;61:1111-1112.
5. Mallepalli JR, Quinet RJ, Sus R. Eosinophilic fasciitis induced by fire ant bites. Ochsner J. 2008;8:114-118.
6. Hamilton ME. Eosinophilic fasciitis associated with L-tryptophan ingestion. Ann Rheum Dis. 1991;50:55-56.
7. Chun JH, Lee KH, Sung MS, Park CJ. Two cases of eosinophilic fasciitis. Ann Dermatol. 2011;23:81-84.
8. Bischoff L, Derk CT. Eosinophilic fasciitis: demographics, disease pattern and response to treatment: report of 12 cases and review of literature. Int J Dermatol. 2008;47:29-35.
9. Khanna D, Agrawal H, Clements PJ. Infliximab may be effective in the treatment of steroid-resistant eosinophilic fasciitis: report of three cases. Rheumatology (Oxford). 2010;49:1184-1188