“Pickoff” Injury in a Softball Player
An 18-year-old complained of pain and decreased mobility of the small finger in his right hand after a softballinjury. While sliding back to second base during a pickoff attempt, the patient hit his hand on the bag.


An 18-year-old complained of pain and decreased mobility of the small finger in his right hand after a softball injury. While sliding back to second base during a pickoff attempt, the patient hit his hand on the bag. In the emergency department, the small finger was in a flexed position. There was pain and swelling over the dorsum of the patient’s dominant right hand. The results of anteroposterior (AP) and lateral radiography were read as normal.
The patient’s hand was placed in a volar splint, and he was discharged. The patient was seen in our office 3 days later. He complained of increasing
hand pain, mostly over his small finger. There was significant ecchymosis and swelling over the small finger, which was most tender over the metacarpophalangeal (MCP) joint.
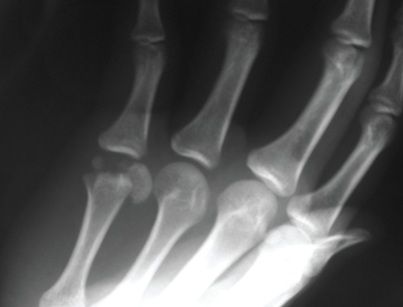
An oblique hand radiograph was obtained in the office. AP (top left), lateral (top right), and oblique (right) x-ray views of the hand are shown here.
What is your diagnosis?
(Find the answer on the next page.)

A displaced intra-articular fracture of the fifth metacarpal head was identified.The fifth is the second most common intra-articular fracture of the metacarpal head; the second metacarpal head is the most common. Sports injuries usually are the cause.
Fractures of the metacarpal head are uncommon. Injury of the second metacarpal is more common because the carpometacarpal (CMC) joint is somewhat immobile; the fifth CMC joint has significantly more motion.With an axially directed force, the second metacarpal head is more at risk for fracture; fracture of the fifth metacarpal neck is more probable because of the flexed position it assumes when there is an axially directed force.
McElfresh and Dobyns1 reviewed 103 metacarpal head fractures; patterns of fracture ranged from collateral ligament avulsions to extensive comminuted fractures. Comminuted head fractures- found in 31 of the 103 patients, most often the result of axially directed forces to the metacarpal
head-were the most common pattern.
Regardless of how benign a hand injury may appear, physicians should take care to evaluate pertinent historical factors and then perform a complete physical and radiographic examination. The patient should be questioned about any initial deformities, bleeding, altered sensation or circulation, and symptoms of sensory or motor disturbance.
Radiographic evaluation of the tubular skeleton of the hand requires 4 views: AP, lateral, and 2 oblique.2 These views allow the physician to assess accurately the position, integrity, and relationship of the many bones that make up the hand. In this case, the oblique view was pertinent in identifying the patient’s fracture.
Intra-articular metacarpal head fractures are especially difficult to identify on lateral radiographs because of overlapping of the MCP joints. CT scans of the hand may help in cases in which the level of clinical suspicion of a fracture is high despite a lack of evidence on plain x-ray films.
For most nondisplaced metacarpal head fractures, closed treatment with early range of motion is adequate. However, late traumatic arthritis is unavoidable when a portion of the head is destroyed or when a congruent joint surface cannot be reestablished. When the articular surface is displaced by more than 1 mm or when more than 20% of the joint is involved, open reduction and internal fixation of the fracture typically is required, as in our patient.


Our patient’s hand was immobilized in a splint; he was taken to the operating room for this procedure. An incision was made centered off the prominence of the metacarpal head on the ulnar aspect of the MCP joint.The fracture fragments were reduced gently and the soft tissues were left in place to minimize the risk of devascularization. Anatomic alignment was restored and fixation was maintained with Kirschner wires, or K-wires. An intraoperative photograph (above) illustrates the displaced and rotated metacarpal head being elevated in an attempt to reduce the fracture for the pinning. Postoperative radiographs illustrate the anatomic reduction of the fractured head. The displaced head is held in place with 2 K-wires traversing the head into the cortex of the metacarpal shaft.
The patient’s finger was immobilized in a cast with K-wires for 4 weeks.Then the wires were removed. An aggressive physical therapy program was started to restore range of motion and strength. The program consisted of both active and active-assisted range of motion exercises that then progressed to passive range of motion of the fifth MCP joint. There were no postoperative complications related to hardware, wound healing, or therapy. The patient progressed without difficulty and ultimately was allowed to return to sports activities after 3 months.

A serious complication of this fracture is avascular necrosis resulting from either the initial trauma or operative intervention.3 A 6-month follow-up x-ray film of the patient’s finger, shown at left, portrays a healed fracture with maintenance of the anatomic reduction that was achieved in the operating room. There is no gross evidence of avascular necrosis or collapse of the articular surface of the metacarpal head. At 1-year follow-up, the patient’s grip strength of the right hand was 110 lb, with full flexion and extension of the small-finger MCP joint.
This case was submitted by Samuel A. Joseph, Jr, MD, assistant clinical instructor in the department of orthopedic surgery at State University of New York (SUNY) at Stony Brook and Winthrop-University Hospital in Mineola, New York, and Glenn A.Teplitz, MD, vice chairman, department of orthopedic surgery, and chief, division of hand services, at Winthrop-University Hospital and assistant clinical professor, department of orthopedics, at SUNY at Stony Brook.
References:
1. McElfresh EC, Dobyns JH. Intra-articular metacarpal head fractures. J Hand Surg. 1983;8A:383-393.2. Lane CS. Detecting occult fractures of the metacarpal head: the Brewerton view. J Hand Surg. 1977;2A:131-133.3. Hastings H 2nd, Carroll C 4th. Treatment of closed articular fractures of the metacarpophalangeal and proximal interphalangeal joints. Hand Clin. 1988;4:503-527.