Abdominal Pain, Vomiting, and Nausea in a 17-Year-Old Patient
A 17-year-old boy presented with a 3-day history of left upper quadrant abdominal pain; intermittent pain radiated to the right side. The patient complained of nonbilious vomiting and nausea and reported subjective fever. He also had a decreased appetite and up to 10 daily bouts of nonmucoid diarrhea.
A 17-year-old boy presented with a 3-day history of left upper quadrant abdominal pain; intermittent pain radiated to the right side. The patient complained of nonbilious vomiting and nausea and reported subjective fever. He also had a decreased appetite and up to 10 daily bouts of nonmucoid diarrhea.
The patient had no history of sick contacts or recent travel. He reported occasional use of recreational drugs.
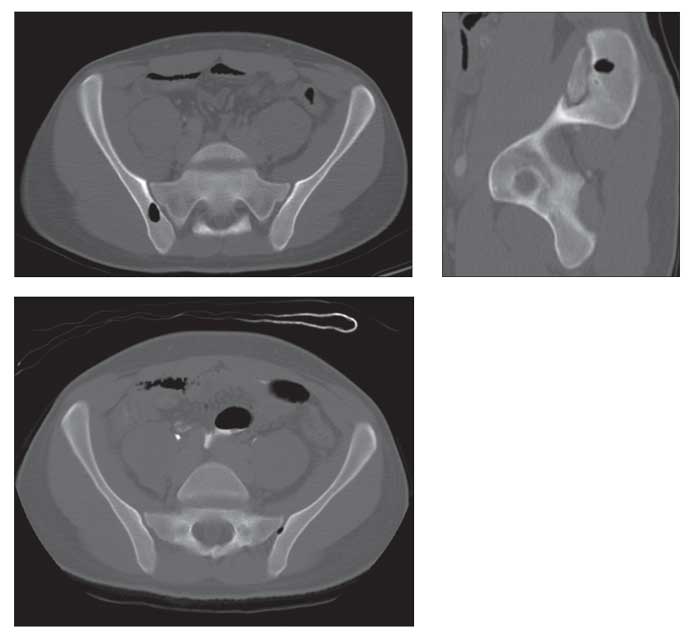
Contrast-enhanced CT scanning of the patient’s abdomen and pelvis showed enterocolitis. On evaluation of the bones, a well-defined lucent lesion measuring between −896 and −913.7 Hounsfield units, isodense to bowel gas and consistent with air attenuation, was noted within the right ilium abutting the superior aspect of the right sacroiliac joint (top, left and right images). This lesion measured 1.4 × 0.97 × 1.4 cm. The right sacroiliac joint was normal. A tiny lucency of air attenuation was projecting over the superior aspect of the left sacroiliac joint, characteristic of “vacuum phenomenon” (bottom). No other bony abnormalities were identified.
The patient was admitted to the pediatric ward, and intravenous hydration was started. Stool cultures from the day of admission were positive for Salmonella. During the patient’s 2-day hospital stay, his symptoms improved and the diarrhea and vomiting resolved. The patient was not aware of any musculoskeletal symptoms.
What is your diagnosis?
(Find the answer on the next page.)
The diagnosis was incidental intraosseous pneumatocyst of the ilium. A gas-containing, cyst-like lesion within the medullary cavity of the bone, intraosseous pneumatocyst is a rare benign lesion reported primarily in the adult population. The lesion has been described most frequently adjacent to joints, especially the sacroiliac joint.
Intraosseous pneumatocysts related to the sacroiliac joint have a predilection for the iliac side of the joint, theoretically because of differences in the characteristics of the surrounding cartilage. The iliac bone is lined by fibrocartilage that is thin compared with the almost twice as thick sacral hyaline cartilage,1 facilitating diffusion of gas into the iliac bone. Intraosseous pneumatocysts have been reported in many sites, including vertebral bodies-especially cervical vertebrae-as well as the clavicle, rib, acetabulum, and scapula.
The cause of pneumatocysts is unclear, but several theories have been suggested. Ramirez and colleagues2 proposed that there is spontaneous development of intraosseous air or gas accumulation within a preexisting simple fluid-filled cyst or ganglion. Yamamoto and associates3 described a case of a cervical pneumatocyst in which an air-filled cyst became a fluid-filled cyst and subsequently was replaced with granulation tissue, as shown by MRI at 40 weeks’ follow-up. Laufer and colleagues4 suggested that the collection of gas is actually nitrogen and is released from the adjacent joint.
Vacuum phenomenon in and of itself refers to the presence of nitrogen gas; typically, it is noted in the intervertebral disks, where it occurs in conjunction with degenerative disease. Vacuum phenomenon also can be induced in normal joints with traction, which creates a negative pressure state in the joint and thereby elicits the release of nitrogen gas from adjacent soft tissues into the joint.
Although acquired benign air cysts in bone have been reported in proximity to joints with degenerative changes and vacuum phenomenon, no underlying joint disease was present in other reports of cases. Berenguer and coworkers5 reported cases of sacral pneumatocysts in patients in whom there were findings of degenerative changes of the joint along with intra-articular gas.
These gas collections in the bone may progress in size or to fluid-filled cysts.3 Hall and Turkel6 observed an adult patient who had a normal ileum on CT examination before decompression of an S1 nerve root and L4, L5, and S1 fusion. A follow-up study performed 2 years later incidentally revealed a pneumatocyst that enlarged on a follow-up study 6 years later. This case illustrates the acquired nature of pneumatocysts. Other reports in the literature describe pneumatocysts that did not change in size on follow-up imaging 6 months to 2 years after the initial imaging.
Intraosseous pneumatocyst is a rare finding in the pediatric population. Kota and Coleman7 described well-defined intraosseous gas with sclerotic margins in the ileum of a 9-year-old boy in whom a CT scan was obtained because of a history of blunt trauma and abdominal pain. In our present case, however, the patient had no recent or remote history of trauma.
Another case report described an intraosseous pneumatocyst in a right cervical rib in a 17-year-old girl who had Klippel-Feil syndrome.8 There was no history of trauma, and a lack of weight bearing associated with this bone makes the pathogenesis of this lesion less likely to be associated with degenerative joint disease. As in our case, these lesions often are asymptomatic and usually are an incidental finding on imaging performed for another disease process.
On plain radiography, pneumatocysts appear as lucent areas with sclerotic margins projecting over an osseous structure. Although occasionally they are visible, plain radiography has its limitations. The small size and location of the lesion are variables that affect the sensitivity of plain radiography.
CT is the most helpful modality in making this diagnosis. CT has greater contrast resolution and high sensitivity for gas collections, even when they are small.6 The CT scan demonstrates the gas density within the medullary cavity of the bone and its borders and documents precisely the size and location of the lesion in the bone and its proximity to the joint.
On MRI, intraosseous pneumatocysts show low signal on T1- and T2-weighted images with no enhancement on contrast-enhanced T1-weighted pulse sequences.9 Bone scintigraphy performed in 2 cases did not identify these lesions.2,6
Intraosseous pneumatocyst is a rare, asymptomatic, benign entity that can occur in association with degenerative joint disease and vacuum phenomenon or as an isolated idiopathic finding. The lesion resides in subchondral bone, and the sine qua non is gas attenuation in bone. Other entities that can present with intraosseous gas include postsurgical and posttraumatic states, anaerobic osteomyelitis, ischemic osteonecrosis, osteoarthritis, osteochondrosis, neoplasm, and microtrauma in patients with osteoporosis.
Recognizing intraosseous pneumatocysts and distinguishing them from other gas-containing intraosseous lesions seen in various clinical settings is essential. The presence of an incidental intraosseous gas collection surrounded by a sclerotic rim or demonstrating well-circumscribed borders is pathognomonic for intraosseous pneumatocyst, which requires no follow-up, biopsy, or surgical intervention.
Comments about/problems with this article? Send feedback.
References:
1. McLauchlan GJ, Gardner DL. Sacral and iliac articular cartilage thickness and cellularity: relationship to subchondral bone end-plate thickness and cancellous bone density. Rheumatology (Oxford). 2002;41:375-380.
2. Ramirez H Jr, Blatt ES, Cable HF, et al. Intraosseous pneumatocysts of the ilium: findings on radiographs and CT scans. Radiology. 1984;150:503-505.
3. Yamamoto T, Yoshiya S, Kurosaka M, et al. Natural course of an intraosseous pneumatocyst of the cervical spine. AJR. 2002;179:667-669.
4. Laufer L, Schulman H, Hertzanu Y. Vertebral pneumatocyst: a case report. Spine (Phila Pa 1976). 1996;21:389-391.
5. Berenguer J, Pomés J, Bargalló N. Sacral pneumatocysts: CT appearance. J Comput Assist Tomogr. 1994;18:95-97.
6. Hall FM, Turkel D. Case report 526: intraosseous pneumatocyst of the ilium. Skeletal Radiol. 1989;18:127-128.
7. Kota G, Coleman L. Clinical image. Air in bone: intraosseous pneumatocyst in a child. Pediatr Radiol. 2006;36:999.
8. Haktanir A, Degirmenci B, Albayrak R, et al. Klippel-Feil syndrome associated with pneumatocyst of the right cervical rib. South Med J. 2005;98:1132-1134.
9. Karasick D, Eason MA. Vertebral pneumatocyst mimicking susceptibility artifact on MR imaging. AJR. 1998;170:221.