Majority of Patients With Juvenile Idiopathic Arthritis Achieved Clinical Remission
“Juvenile idiopathic arthritis constitutes a significant cause of disability and quality of life impairment in pediatric and adult patients,” investigators stated. “Recent advances in JIA treatment addressing more specific targets have led to better short and long-term disease outcomes."
Over two-thirds of patients with juvenile idiopathic arthritis (JIA) attained clinical remission (CR), with females who exhibited lower active joint count and antinuclear antibody (ANA) positivity more likely to achieve and sustain remission, according to a study published in Pediatric Rheumatology.1
“Juvenile idiopathic arthritis constitutes a significant cause of disability and quality of life impairment in pediatric and adult patients,” investigators stated. “Recent advances in JIA treatment addressing more specific targets have led to better short and long-term disease outcomes. Nevertheless, a notable proportion of patients relapse, either while still on medication or after its withdrawal.”
In this single-center, retrospective-prospective, observational study, investigators analyzed patients with JIA who attended Vall d’Hebrón University Hospital’s Pediatric Rheumatology Unit and were treated with synthetic and/or biological disease-modifying antirheumatic drugs (DMARDs). The primary outcome was the percentage of patients who achieved clinical remission on and off medication. DMARD treatment was subdivided into 4 groups: synthetic DMARD (sDMARD), sDMARD with another sDMARD, sDMARD with a biologic DMARD (bDMARD), and those receiving bDMARD therapy alone. A 2-year prospective follow-up was performed, and patients were evaluated every 3 months using study protocol.
Data such as demographics, clinical, immunologic, and medications were recorded from medical records.
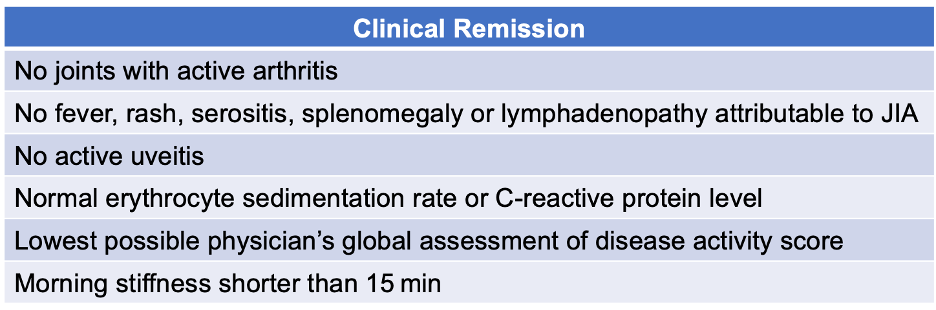
CR on medication was defined as the above criteria being fulfilled for at least 6 months. Patients achieving CR off medication sustained CR for at least 12 months after medication was withdrawn.
The cohort was 71% female, 93% White, 52% had an oligoarticular JIA, and patients had a median age at disease onset of 3 years.
A total of 206 patients with JIA receiving DMARDs were analyzed, with 70% of patients (144 out of 206) achieving CR at least once and 29% (59 out of 206) were in CR without medication. Patients receiving sDMARDs alone were more likely to achieve CR (53%). Within this subcategory, it was more likely observed in female patients with ANA positivity and oligoarticular persistent subtypes. Relapse rates were lower in patients with persistent oligoarticular JIA (93%) when DMARDs were tapered before withdrawal (77%). Dose tapering was performed in 66% of patients observed.
After further exclusions, 159 patients were included in the prospective study, receiving 267 DMARDs. CR was achieved in 17% (27/159) patients during the 2-year follow-up study. Throughout the follow-up period (a median time of 7 years), 136 patients remained on treatment. Of patients who achieved CR at least once, 94% were White, 84% had persistent oligoarticular JIA, and 75% did not have a history of DMARD-related adverse events.
DMARDs were tapered in 74% of patients and only 11% had a relapse during this time. Of the 267 treatments administered, 34% achieved CR and were withdrawn, with a median treatment to withdrawal of 12 months. A total of 69% of patients were able to maintain this through the 24-month prospective study period.
The study was limited by its design, which may have led to selection bias and a reduced number of patients. Thus, generalizability may be inherently hindered. Additionally, the total duration of CR for patients on and off medication was unavailable.
“In patients who already have attained remission, a progressive DMARD dose tapering for at least 1 year before considering withdrawal would minimize the probability of subsequent relapse, particularly in those who required a biologic DMARD to achieve a quiescent state of the disease,” investigators concluded.
Reference:
Castillo-Vilella M, Giménez N, Tandaipan JL, Quintana S, Modesto C. Clinical remission and subsequent relapse in patients with juvenile idiopathic arthritis: predictive factors according to therapeutic approach. Pediatr Rheumatol Online J. 2021;19(1):130. Published 2021 Aug 21. doi:10.1186/s12969-021-00607-0