Pharmacogenetics in Rheumatology: Disappointment, Success, and a Few Challenges
Both genetic science and drug development are advancing rapidly against rheumatologic disease. Is pharmacogenetics keeping pace? Here is an update, authored by a rheumatologist expert from Washington University School of Medicine.
Over the last decade, there have been rapid advances in the pharmacogenetics of drugs used in rheumatology. In the near future, pharmacogenetic applications to traditional disease-modifying anti-rheumatic drugs (DMARDs) such as methotrexate and the newer biological agents may set the stage for individualized therapy in the rheumatic diseases. However, although pharmacogenetics has moved rapidly toward the clinic in other fields, notably oncology and psychiatry, its progress in rheumatology has not matched the pace of recent drug development, for several reasons enumerated below.
Pharmacogenetics is the study of variations such as single nucleotide polymorphisms (SNPs) in genes that encode drug transporters, drug-metabolizing enzymes, and drug targets, and their association with drug effects such as efficacy and toxicity. Beginning with examples of two drugs in rheumatology, whose pharmacogenetics is established in one case and exploratory in the other, this brief update provides a perspective on the current status and future directions of the field as applied to rheumatology.
Methotrexate (MTX), the ‘gold standard’ drug in rheumatoid arthritis (RA), exerts its anti-inflammatory effects by inhibiting enzymes in the cellular folate and adenosine pathways. A multitude of polymorphisms in genes encoding these enzymes (including those in RFC1, ABCB1, FPGS, GGH, DHFR, MTHFR, SHMT, TYMS, and ATIC) have been examined for their effects on MTX efficacy and toxicity in RA.1
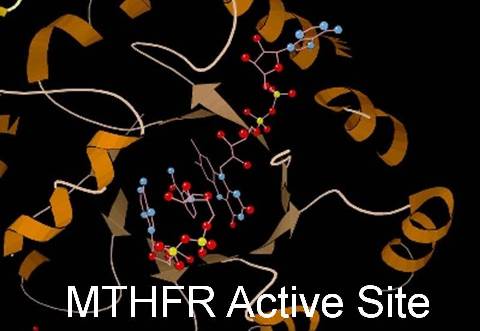
Among these, two SNPs in the gene that codes for a key enzyme in the folate pathway, methylene tetrahydrofolate reductase (MTHFR), are functional in that they alter the activity of the encoded protein. These SNPs (named 677C>T and 1298A>C) have been the most well-studied. However their influence on the response to MTX remains equivocal, as demonstrated by numerous studies and two meta-analyses.
One showed an association between the SNP 677C>T (but not 1298A>C) and MTX toxicity.2 Another recent meta-analysis found no association between either SNP and MTX efficacy or toxicity.3 As no clear genetic markers have emerged that can predict therapeutic outcomes with this drug, the pharmacogenetics of MTX in rheumatology remain exploratory.
Azathioprine (AZA), in contrast, benefits from an established pharmacogenetic test that is already in wide clinical use in rheumatology and is recommended in the package insert for the drug. Despite the availability of newer biological agents such as rituximab and belimumab, AZA remains an important drug in the treatment of systemic lupus erythematosus (SLE).
AZA is converted after a series of intermediate steps to cytotoxic thioguanine nucleotides, which can cause hematopoietic and gastrointestinal toxicity. (It is also converted to inactive metabolites, the methylmercaptopurine nucleotides.) Patients homozygous or heterozygous for any of the variant alleles of the gene TPMT, which codes for the enzyme thiopurine methyltransferase (the enzyme that inactivates the cytotoxic thioguanides), are at high risk for these toxic
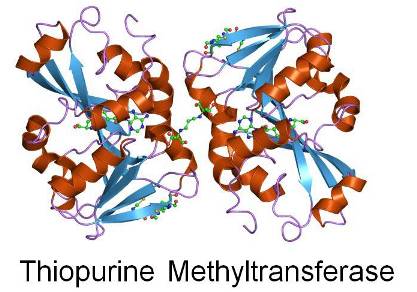
adverse events.4-6 Three variants in the TMPT gene (TPMT*2, TPMT*3A, and TPMT*3C) are responsible for intermediate or low activity of TMPT.
Because of the existence of these variants, there is considerable variability among individuals in erythrocyte TPMT activity. Most people (90%) have normally high activity of the enzyme, but 10% have intermediate activity and 0.3% have low or no activity. The TPMT genotyping assay, used before initiating the drug to assess an individual patient’s risk for AZA toxicity, is an example of the effective application of pharmacogenetics in rheumatology.
Present status and future directions
In addition to MTX and AZA, the pharmacogenetic properties of several other drugs used in the treatment of rheumatic diseases (including hydroxychloroquine, sulfasalazine, leflunomide, cyclophosphamide, and the biological agents such as the anti-tumor necrosis factor agents) are under investigation.7 Despite a multitude of studies and variants analyzed, with the exception of AZA the field remains muddled. No single variant has emerged consistently as a predictor of drug efficacy or toxicity to allow the development of a clinically useful pharmacogenetic assay.
The reasons for this are manifold. Among them:
• Diseases such as RA and SLE are complex and polygenic, with wide variability in phenotypes (clinical presentation) and genotypes. This prevents the easy classification of patients based on their predicted drug response.
• Drugs used to treat the rheumatic diseases typically affect not one but several genes and pathways. Determining only a few variants in these genes and pathways may not be fruitful. Examination of haplotypes and/or multi-gene signatures in candidate gene regions (such as TNF and MTHFR) rather than individual SNPs may be more useful.
• Synovial tissue is seldom obtained and available for analysis. As the "target" of inflammatory arthritis, synovial tissue may be the most high-yield tissue for genetic studies. But such an approach is not often feasible because the cells that may be most informative about response to a drug are not available to be assessed pharmacogenetically.
• Most pharmacogenetic studies in rheumatology have been performed with small sample sizes, in racially homogeneous populations, with a few exceptions.8 This limits the external validity of these studies. Large, multi-racial cohorts need to be studied.
Despite these caveats, and the fact that pharmacogenetics in rheumatology is still in its infancy, this is a fast-growing field. Continued research should soon make individualized drug therapy in the rheumatic diseases a reality.
(For References, scroll beyond the Comments box below.)
References:
REFERENCES:
1. Ranganathan P, McLeod HL. Methotrexate pharmacogenetics: the first step toward individualized therapy in rheumatoid arthritis.Arthritis and Rheumatism (2006): 54:1366-1377
2. Fisher MC, Cronstein BN. Metaanalysis of methylenetetrahydrofolate reductase (MTHFR) polymorphisms affecting methotrexate toxicity.J Rheumatol. (2009) 36:539-545
3. Owen SA, Lunt M, Bowes J, et al. MTHFR gene polymorphisms and outcome of methotrexate treatment in patients with rheumatoid arthritis: analysis of key polymorphisms and meta-analysis of C677T and A1298C polymorphisms.Pharmacogenomics J. (2013) 13:137-147
4. Kerstens PJ, Stolk JN, De Abreu RA, et al. Azathioprine-related bone marrow toxicity and low activities of purine enzymes in patients with rheumatoid arthritis.Arthritis & Rheumatism (1995) 38:142-145
5. Stolk JN, Boerbooms AM, de Abreu RA et al. Reduced thiopurine methyltransferase activity and development of side effects of azathioprine treatment in patients with rheumatoid arthritis.Arthritis & Rheumatism (1998) 41:1858-1866
6. Higgs JE, Payne K, Roberts C, Newman WG. Are patients with intermediate TPMT activity at increased risk of myelosuppression when taking thiopurine medications?Pharmacogenomics (2010) 11:177-188
7. Davila L, Ranganathan P. Pharmacogenetics: Impact on Therapeutics for Rheumatic Disease.Nature Reviews Rheumatology (2011) 7:537-550
8. Ranganathan P, Culverhouse R, Marsh S et al. Methotrexate pathway gene polymorphisms and their effects on methotrexate toxicity in Caucasian and African American patients with rheumatoid arthritis.Journal of Rheumatology (2008)35:572-579.