Tests and treatments of overuse syndromes: 20 Clinical pearls
"Overuse syndromes" is an umbrella designation that covers a variety of upper extremity disorders, including tendinitis of the hand and wrist and epicondylitis.
"Overuse syndromes" is an umbrella designation that covers a variety of upper extremity disorders, including tendinitis of the hand and wrist and epicondylitis. In many sports and occupational activities, overuse syndromes often result from cumulative, repetitive microtrauma that causes tissue damage. Factors usually considered to contribute to these injuries are repetition or prolonged use, force applied directly to soft tissues, and awkward postures.
Overuse injuries generally are more common in older persons, but they can occur in any age-group; these injuries are increasingly more common in children as this age-group becomes more active in organized sports. Overuse injuries may be the most common category of sports injuries that primary care physicians encounter, accounting for 30% to 50% of sports injuries.1 Repetitive overuse injuries account for roughly half of work-related ailments; these disorders are most commonly seen in the hand, wrist, shoulder, and spine.
Carpal tunnel syndrome (CTS) is commonly seen in the workplace; its prevalence is highest among technicians, machine operators, assemblers, and farmers and in the mining, agriculture, and construction industries.2 CTS also is common in musical instrumentalists and computer users.
Pinpointing a precise diagnosis for an upper extremity overuse syndrome tends to be difficult because occupational syndromes often involve subjective complaints of pain and tenderness. Successful diagnosis begins with a thorough understanding of the relevant anatomy and a working knowledge of examination techniques. A variety of specific tests may help assessment. In this article, I offer 20 practical tips on sorting through the many overuse disorders that can occur in the hand, wrist, and elbow and on determining effective strategies for managing them.
HAND AND WRIST PEARLS
1. Physical findings in carpal tunnel syndrome
Median nerve compression at the wrist, and the CTS that results, is the most common upper extremity nerve compression syndrome and one of the most common problems that physicians who manage musculoskeletal diseases encounter.3,4 Compression of the median nerve occurs within the narrow carpal canal, which is formed by the transverse carpal ligament anteriorly, the hook of hamate ulnarly, the trapezium radially, and the carpal and volar ligaments dorsally (Figure). Nine flexor tendons and the median nerve pass through the carpal tunnel, which is narrowest in its mid portion, where the median nerve can easily become entrapped between the wrist bones and the transverse carpal ligament.
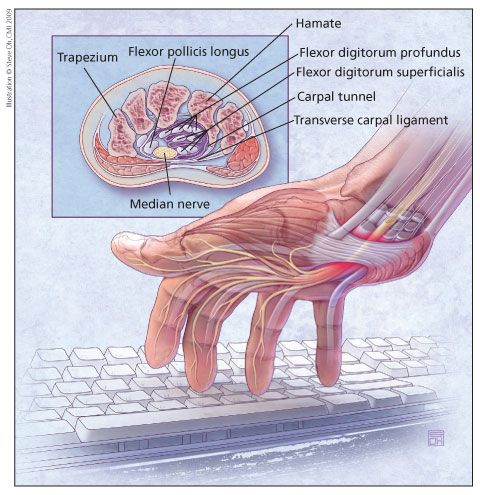
Figure – The most common upper extremity nerve compression syndrome is median nerve compression at the wrist. This occurs within the narrow carpal tunnel, which is formed by the transverse carpal ligament anteriorly, the hook of hamate ulnarly, the trapezium radially, and the carpal and volar ligaments dorsally (inset). The result is carpal tunnel syndrome; the cause may be repetitive stress, physical injury, or an underlying medical or physical problem.
Whether CTS should be considered an overuse injury is controversial. Any process that decreases the volume of the tunnel or increases the volume of the contents may provoke symptoms of median nerve compression. CTS may be caused by repetitive stress; physical injury; or an underlying medical or physical problem, such as pregnancy, diabetes mellitus (DM), rheumatoid arthritis (RA), or obesity. Studies have suggested that more than half of cases of CTS are associated with workplace factors; however, there is no clear evidence of a causal relationship.5
In a case-controlled study, Fung and associates6 evaluated wrist posture, loading, and repetitive motion as risk factors for CTS. They concluded that patients who perform frequent extension and flexion and sustained forceful motions of the wrist are at increased risk for CTS.
Patients may present with complaints ranging from paresthesia throughout the hand to paresthesia only in the long and ring fingers to the more classic distribution in the thumb, index and long fingers, and a portion of the ring finger. The Phalen test and maneuver, in which the wrist is palmar flexed for 30 to 60 seconds, is a provocative test that helps make the diagnosis. A positive result consists of elicitation of paresthesia and reproduction of the patient's symptoms.
Other tests are the direct median nerve compression test, in which a positive result is an increase in pain and paresthesia with direct compression of the median nerve for 30 seconds, and the Tinel sign, in which paresthesia is felt in response to local percussion over the median nerve at the carpal tunnel. Two-point discrimination, grip strength, and thenar muscle function also should be checked.
2. Management of carpal tunnel syndrome
Factors to consider in determining treatment of patients with CTS include the length of time the patient has had symptoms and the severity of symptoms. Initial treatment includes splinting and, in cases of acute CTS, NSAIDs. Forearm flexibility and strengthening exercises also may be used for therapy. Because CTS is a common complaint in workers who are performing repetitive activities, an ergonomically beneficial workstation might be recommended.
If the patient has been symptomatic for less than 6 months, a corticosteroid/local anesthetic injection in the carpal canal may be tried. Injection is performed directly over the transverse reticular ligament radial to the ring ray. Care must be taken to avoid intraneural injections (continually ask the patient whether paresthesias are occurring and, if so, retract the needle). I use a 25-gauge needle and inject 1 mL of 1% xylocaine, 1 mL of bupivacaine, 0.5 mL of dexamethasone, and 0.5 mL of betamethasone.
In a systematic review of randomized clinical trials on conservative treatment of patients with CTS, Piazzini and colleagues7 found strong evidence to support the efficacy of local and oral corticosteroids, moderate evidence of support for the effectiveness of splints, and moderate evidence that vitamin B6 is ineffective. Conflicting evidence was found in terms of the efficacy of NSAIDs, diuretics, yoga, laser, and ultrasonography. Evidence for the ineffectiveness of botulin toxin B injections and exercise therapy was conflicting.
3. Detecting chronic scapholunate insufficiency
The scapholunate ligament maintains the proximal pole of the scaphoid adjacent to the lunate and stabilizes the palmar rotation force of the scaphoid against the dorsal rotation force of the lunate. In scapholunate insufficiency, the whole scaphoid rotates palmarly and the proximal pole subluxates dorsally, creating a rotatory subluxation of the scaphoid. Instability of the scaphoid results in cartilage damage in the scaphoid fossa at the radial styloid process.
Much has been said about the value of the scaphoid shift, or Watson, test in making the diagnosis. It is designed to detect abnormal motion between the scaphoid and the lunate resulting from damage to the scapholunate ligament; the result is considered positive if pain and scaphoid subluxation on the radius are elicited.
The test is performed by exerting dorsal pressure on the distal pole of the scaphoid as the wrist is ulnarly and radially deviated. As ulnar deviation occurs, the scaphoid is raised above the level of the dorsal lip of the radius; when radial deviation occurs, it snaps back into place. The examiner should perform the test with the same-side hand as is injured in the patient.
The test results must be looked at in the clinical context. Many persons have a positive scaphoid shift bilaterally just because of congenital laxity of the ligaments. Therefore, the contralateral wrist always should be checked and the test results may be symmetrical; this does not point to a diagnosis of scapholunate ligament insufficiency. If there is a history of trauma and a unilateral positive scaphoid shift, this is an excellent indicator of the entity.
4. Dorsal wrist syndrome
This syndrome usually is the result of a mild injury to the scapholunate ligament and, occasionally, the presence of an occult dorsal wrist ganglion. Physical findings may include point tenderness over the dorsal aspect of the scapholunate region of the wrist and pain with passive dorsiflexion. Dorsal wrist syndrome may be distinguished from a scaphoid injury by the localized tenderness.
One important point in the examination is to have the patient try to lift himself or herself off the table from a sitting position with the wrist in dorsiflexion. If dorsal wrist syndrome is present, he most certainly will have pain or the inability to perform this maneuver.
5. Diagnosis of pain at the base of the thumb
Pain at the base of the thumb or radial aspect of the wrist is a common complaint. The most common diagnoses are basilar joint arthrosis and de Quervain syndrome. These entities are easily distinguished by clinical examination.
Basilar joint arthrosis occurs at the trapezial first metacarpal joint. This condition is commonly indicated by tenderness over the basilar joint and a positive "grind test," in which axial load is placed on the thumb and the trapezial first metacarpal joint is compressed, or "shucked," as the axial load is administered. This causes grinding and reproduces the patient's pain in cases of trapezial first metacarpal arthritis.
De Quervain syndrome, one of the most common types of tendon lining inflammation, results from compression of the first dorsal compartment tendons-the abductor pollicis longus and extensor pollicis brevis tendons. The swollen tendons and their coverings cause friction within the narrow tunnel or sheath through which they pass, resulting in pain at the radial styloid.
Pain along the back of the thumb, directly over the 2 thumb tendons, is typical. The condition can occur gradually or suddenly; the pain may travel into the thumb or up the forearm. Thumb motion may be difficult and painful, particularly with pinching or grasping of objects. Overuse, a direct blow to the thumb, repetitive grasping, and inflammatory conditions can trigger the disease. Often, the cause is unknown.
6. Stenosing tenosynovitis of flexors of the digits and thumb
This condition, also known as trigger finger or trigger thumb, results from nodular thickening of the flexor tendon within the distal aspect of the palm. The condition is a common abnormality in patients with DM or RA, particularly patients in middle age or older. Patients usually present with pain in the flexor sheaths of digits or thumb flexors and frequently complain of catching or triggering of the digits. This is common in the morning upon arising. Sometimes, the tendon becomes entrapped proximal to the annular (A-1) pulley when the digit is flexed.
Initial treatment usually includes icing and injection of corticosteroid into the sheath; 70% to 80% of patients respond, at least temporarily.8 If the condition recurs, either a second injection or surgical decompression of the A-1 pulley may be considered.
7. Ulnar impaction syndrome
Ulnar wrist pain is a common complaint; a good understanding of the many possible causes helps in making the diagnosis. Diagnoses range from extensor carpi ulnaris tendinitis to subluxation of the extensor carpi ulnaris to hook of hamate fracture to triangular fibrocartilage tear to ulnar carpal impingement. The diagnosis should be based on the history, especially if there was a single traumatic event that seemed to initiate the pain or a chronic progression of pain.
Ulnar carpal impingement or impaction usually is the result of a congenital positive ulnar variance in which the distal ulna is slightly longer (normally 1 to 2 mm) than the distal radius. This discrepancy places extra stress on the ulnar side of the wrist, possibly leading to chronic tearing of the triangular fibrocartilage and pain. X-ray films should be obtained initially, including posteroanterior (PA), 0 rotational PA, and lateral views (wrist in neutral rotation).
8. Extensor carpi ulnaris tendinitis of the wrist
Soft tissue injuries of the hands and wrists are common in participants in racket sports because the racket handle has a direct impact and repetitive stretching occurs as the wrist is forcefully whipped into extremes of positions. Tendinitis can occur in all tendons but is most common in the first dorsal compartment, flexor carpi ulnaris, flexor carpi radialis (FCR), and extensor carpi ulnaris.
Extensor carpi ulnaris tendinitis is seen frequently in the nondominant wrist of tennis players who use a 2-handed backhand. Testing for tenderness over the course of the tendon should be performed by supinating the wrist and having the patient extend the wrist. In supination, the tendon lies radial to the head of the ulna and is easily palpated.
Subluxation of the extensor carpi ulnaris is common in golfers and tennis players. The diagnosis can be made by palpating the tendon with the wrist and forearm in supination and asking the patient to actively ulnarly deviate the hand. This results in the tendon popping over the head of the ulna. The diagnosis can be confirmed by injecting the sheath of the extensor carpi ulnaris with local anesthetic; in both tendinitis and subluxation, this relieves the symptoms.
9. Flexor carpi radialis tunnel syndrome
The FCR tendon travels in its own sheath adjacent to the carpal tunnel. This syndrome, tendinitis of the insertional or distal 2 to 3 cm of the tendon, is rare. The physical findings are point tenderness over the distal aspect of the tendon and pain reproduced by wrist flexion against resistance. Diagnostic tests usually show normal results; a diagnosis may be confirmed by injection of local anesthetic in the FCR tunnel. Frequently, this tendinitis resolves with icing, stretching, and splinting or injection. Occasionally, surgical release of the FCR tunnel is indicated.
10. Intersection syndrome
This fairly common overuse cause of distal forearm pain is inflammation at the point where the abductor pollicis longus and extensor pollicis brevis tendons cross over the extensor carpi radialis longus and extensor carpi radialis brevis tendons in the wrist. Intersection syndrome often is seen in laborers who perform repetitive dorsiflexion of the wrist and in athletes, such as rowers, who do repetitive extension activities. The area of inflammation is about 6 to 8 cm proximal to the radial styloid. Usually, there is associated swelling and point tenderness and, of note, crepitus with active extension of the wrist. Intersection syndrome usually responds quite readily to splinting, rest and, occasionally, injections of corticosteroids.
11. Stress fractures of the hook of hamate
Although somewhat uncommon, this overuse syndrome is seen in participants in golf, tennis, and baseball. The butt end of the racket, club, or bat impacts the hypothenar eminence and injures the hook of hamate. This problem should be suspected in anyone who has a history of chronic pain over the hypothenar area and then suddenly is unable to perform his sports activity or grip an object without pain.
The hook of hamate lies in a line from the pisiform to the head of the second metacarpal about 2 to 3 cm distal to the pisiform. Physical findings include point tenderness over the hook of hamate and significant grip strength weakness. Frequently, plain x-ray film results are normal, but the diagnosis may be made by CT scan with or without a bone scan.
ELBOW PEARLS12. Physical findings in lateral epicondylitis
This common condition is an inflammation or degeneration of the tendon fibers that attach the forearm extensor muscles to the outside of the elbow. Routine use of the arm or an injury to this area may stress or damage the muscle attachment and cause symptoms. Generally, persons in whom lateral epicondylitis develops are involved in activities with motion of the wrist and arm or lifting with the palm side of the hand facing down. The problem is also known as "tennis elbow" because sometimes it occurs in persons who play racket sports.
The most reliable physical findings are point tenderness over and just anterior to the lateral epicondyle and pain with resisted wrist extension with the elbow extended. The point of maximum tenderness should be quite precise.
13. Monitoring patients with lateral epicondylitis
We monitor the course of lateral epicondylitis by using a dynamometer to measure grip strength. Strength is tested with the elbow flexed and extended, and comparison is made with the opposite extremity. Normally, the grip is slightly stronger when the elbow is in extension rather than in flexion. Patients with lateral epicondylitis exhibit a weaker grip with the elbow extended. The clinician can monitor the course of this overuse syndrome by quantitating grip strength at the first visit and then checking it periodically.
14. Management of lateral epicondylitis
We generally recommend initiating treatment by means of icing, stretching, and eccentric wrist strengthening of the extensors. Patients wear a short-arm wrist cock-up splint at night and, occasionally in acute cases, during the day. Splinting relieves stress at the origin of the extensor carpi radialis brevis tendon by limiting wrist flexion. We also use a counterforce brace to relieve the stress from the insertion of the brevis tendon on the lateral epicondyle. We do not recommend injections as an initial therapy because this occasionally results in transient improvement and more difficulty in providing treatment when the condition recurs.
15. Physical findings in medial epicondylitis
The muscles that flex the wrist originate at the medial epicondyle. Forceful and repeated bending of the wrist and fingers causes tiny ruptures of the muscle and tendons in this area. Far less common than lateral epicondylitis, medial epicondylitis is caused by a variety of activities, but primarily golfing. It is commonly referred to as "golfer's elbow." During the golf swing, the flexor muscles and tendons must tighten to hit the ball.
The most common physical finding in the diagnosis of medial epicondylitis is point tenderness at or slightly anterior to the medial epicondyle. The medial epicondylitis, or golfer's elbow, test confirms this finding. With the patient's forearm fully supinated and the wrist completely extended, the examiner passively extends the patient's elbow. Pain in the wrist flexors, frequently at their origin at the medial epicondyle, is an abnormal result. Pain is experienced with adduction of the forearm against resistance.
16. Ulnar collateral ligament insufficiency of the elbow
The ulnar collateral ligament (UCL) originates at the posterior distal aspect of the medial epicondyle of the humerus and inserts into the base of the coronoid process of the ulna. It consists of 3 distinct parts, the anterior, posterior, and transverse bundles.
The UCL, critical for valgus stability of the elbow, is the primary elbow stabilizer. The anterior band, arising from the anteroinferior surface of the medial epicondyle and inserting on the sublime tubercle of the ulna, provides the major contribution to valgus stability. The UCL plays an important role in most throwing sports and some racket sports that involve repetitive overhead activities. UCL injuries are common in young athletes and generally are chronic problems; symptoms include persistent pain and instability.
In my experience, demonstrating instability in the elbow in valgus stress in cases of chronic UCL insufficiency-as seen in the dominant arm of throwers-is difficult. The most diagnostic finding is revealed by the milking-sign or moving valgus stress test.
17. Cubital tunnel syndrome
This syndrome occurs as the ulnar nerve is compressed when it passes through the cubital tunnel posterior to the medial epicondyle of the elbow. It may be caused by trauma; repetitive use of the elbow; or continuous use of the elbow in a flexed position, which stretches and irritates the nerve.
Patients with this syndrome usually present with paresthesia or hypesthesia in the small and ring fingers and, occasionally, grip weakness. In my experience, the elbow flexion stress test is one of the more reliable tests. The elbow is held in acute flexion to see whether this reproduces the symptoms and checked to see whether there is a Tinel sign. Ulnar motor function also should be evaluated.
Initially, we recommend that the patient avoid holding the elbow acutely flexed, such as when talking on the telephone for an extended period. We occasionally prescribe a night splint to keep the elbow at 45° of flexion overnight.
18. Radial tunnel syndrome
This syndrome is an entrapment or compression of the posterior interosseous nerve within the forearm that causes weakness of the muscles supplied by the nerve and pain around the elbow.
The nerve is further stretched and irritated by repetitive forceful pushing and pulling, bending of the wrist, gripping, and pinching. Sometimes a direct blow to the lateral side of the elbow affects the radial nerve.
Radial tunnel syndrome is sometimes confused with lateral epicondylitis. The 2 conditions may coexist in rare cases, but normally there is a significant difference in the physical findings.
19. Evaluation of nerve compression syndromes
When evaluating a patient for a possible nerve compression syndrome, the clinician should perform a thorough examination of the upper extremity from the neck distally. The Spurling test (neck extension and tilting the head toward the involved side, followed by axial compression) is performed to determine whether there is nerve root compression in the neck. The results are abnormal if axial loading by the examiner's hands reproduces symptoms.
Thoracic outlet syndrome (pain, numbness, tingling, or weakness in the arm and hand resulting from pressure against the nerves or blood vessels that supply the arm) can be tested with an Adson maneuver or Roos test. The Adson maneuver is performed with the neck flexed to the opposite side and the shoulder abducted and extended to see whether this produces numbness and tingling in the fingers. A positive Roos sign is seen when abduction and external rotation of the shoulder for 3 minutes causes pain, fatigue, and paresthesia in the ulnar nerve distribution.
20. Diagnostic injections
These can help pinpoint the pathology in various overuse syndromes of the wrist and elbow, particularly in radial tunnel syndrome, where no other diagnostic test results are usually positive. An injection of lidocaine and bipuvicaine hydrochloride in the area of the radial tunnel 3 cm lateral to the biceps tendon is an excellent aid in making the diagnosis.
References:
References1. Herring SA, Nilson KL. Introduction to overuse injuries. Clin Sports Med. 1987;6:225-239.
2. Dillon C, Petersen M, Tanaka S. Self-reported hand and wrist arthritis and occupation: data from the US National Health Interview SurveyâOccupational Health Supplement. Am J Ind Med. 2002;42:318-327.
3. Omer G Jr. Median nerve compression at the wrist. Hand Clin. 1992;8:317-324.
4. Rayan G. Preface of nerve compression syndromes. Hand Clin. 1992;8:21.
5. Falkiner S, Myers S. When exactly can carpal tunnel syndrome be considered work-related? ANZ J Surg. 2002;72:204-209.
6. Fung BK, Chan KY, Lam LY, et al. Study of wrist posture, loading and repetitive motion as risk factors for developing carpal tunnel syndrome. Hand Surg. 2007;12:13-18.
7. Piazzini DB, Aprile I, Ferrara PE, et al. A systematic review of conservative treatment of carpal tunnel syndrome. Clin Rehabil. 2007;21:299-314.
8. Marks MR, Gunther SF. Efficacy of cortisone injection in treatment of trigger fingers and thumbs. J Hand Surg. 1989;14A:722-727.