Wearable technology provides ready-made monitoring for musculoskeletal rehabilitation
Musculoskeletal rehabilitation student researchers at the Spaulding Rehabilitation Hospital in Boston are developing wearable monitoring systems that will allow physicians to monitor patient activity and physiology remotely over extended periods.
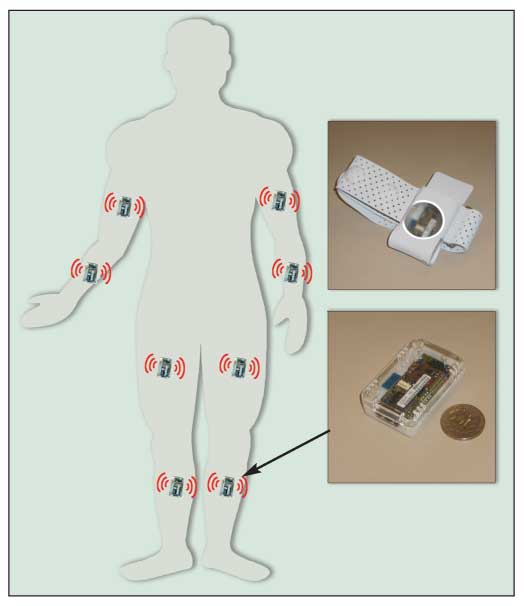
Musculoskeletal rehabilitation student researchers at the Spaulding Rehabilitation Hospital in Boston are developing wearable monitoring systems that will allow physicians to monitor patient activity and physiology remotely over extended periods. Physical rehabilitation–oriented wearable technology research involves the design of minimally obtrusive sensors that can gather, record, and relay information about a patient's physical movements or physiological state, according to Harvard Medical School professor and Spaulding's motion analysis lab director Paolo Bonato, PhD. It also promotes the development of algorithms for extracting information from raw sensor data and providing clinically relevant feedback. Clinicians will be able to assess the impact of physical rehabilitation interventions on patients' lives without interfering with their activities of daily living (ADLs).
A common cause of movement disorder, Parkinson disease (PD) is characterized by tremor, slowness of movement, and impaired postural balance. Dopamine augmentation/replacement therapy has proved effective in managing PD symptoms, but its long-term use is correlated with changes in brain function that cause dyskinesia. In addition, patient habituation to the dopaminergic drugs tends to manifest in an abrupt loss of efficacy at the end of each dosing interval.
To assess efficacy and adverse effects, physicians currently rely on patient self-reports and diaries or on short-term clinical observation. However, these approaches are burdensome and subject to perceptual and recall bias.
Clinical assessments tend to be more accurate but may be equally burdensome and represent only a fraction of the patient's daily experience. Past attempts at using remote sensors proved unsuccessful-the technology was neither reliable nor sensitive enough to capture the data needed for clinical applications, and the amount of data required made storage and transmission problematic.
Recent advances in miniature monitoring systems have made wearable technology more reliable and sensitive for capturing patient movement characteristics associated with symptoms. Student researcher Shyamal Patel's project is a wireless wearable monitoring system that accurately tracks changes in the severity of symptoms in patients with PD. Patel developed procedures that allow for processing of the clinical information at the sensor level and decrease the amount of data and energy required for transmission.
Patel conducted a pilot study with a team led by John Growdon, MD, in the neurology division at Massachusetts General Hospital (MGH). Medication intake, adverse effect occurrence, and wearing off (abrupt loss of medication efficacy) were monitored in 12 patients with PD. Based on the initial data, Patel developed signal-processing algorithms optimized for implementation on the networked wireless sensors. Then he used advanced pattern recognition techniques to accurately predict clinically relevant information about the severity of symptoms.
Patel's model will provide clinicians with a tool for designing treatment protocols based on accurate, reliable data representing complex interactions of medications with multiple symptoms monitored over time. The device will facilitate optimal medication titration and minimization of adverse effects in individual patients; it also may serve as an objective measure of longitudinal changes in patient status that occur because of the degenerative nature of PD and may provide a way to collect data during clinical trials for new pharmaceutical and physical therapy treatments.
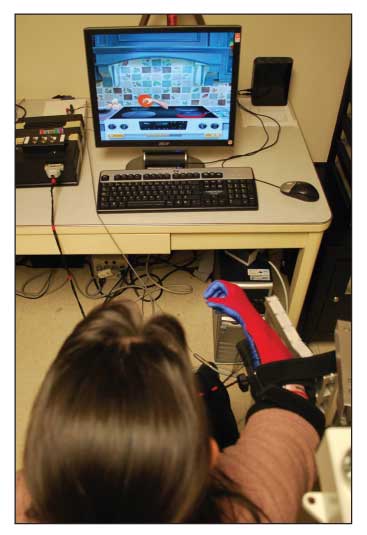
Researchers in neurorehabilitation have explored the repetition of movement patterns that patients with hemiparesis (those experiencing unilateral weakness because of a stroke or a traumatic brain injury) need to "relearn" as a tool for restoring motor function. Wearable sensor technology may prove to be a powerful tool, especially when used with virtual reality and robotics, according to students Fabrizio Cutolo and Chiara Mancinelli.
Virtual reality training platforms offer patients safe, often novel, environments in which they can perform real-life motor tasks, and researchers gain a tool for collecting data on the patients' task performance. The platforms may be designed to include visual, auditory, and haptic feedback and to present patients with alternative motor strategies for completing salient tasks. These features may be essential in motivating patients to perform the high-repetition protocols required for motor skill reacquisition.
Virtual training offers the ideal mental environment for neurorehabilitation; rehabilitation robotics provides the hardware that makes high-intensity, repetitive task performance physically achievable for those with motor deficiencies. Advances in robotic technology have made these devices suitable for facilitating the fine motor skills that tend to elude patients who have neurological conditions. Rehabilitation robotic devices also serve as data collection tools, enabling researchers to create better programs for individual patients.
The hand and finger movements of patients with hemiparesis lack the speed, coordination, accuracy, and force demonstrated in healthy patients-they do not possess the precise motor control required for manipulating objects. In patients with hemiparesis, upper extremity rehabilitation robotic devices may help improve the proximal and fine motor manipulations needed for performing ADLs. In addition, transfer of the learned movements into functional tasks has been observed in patients with various degrees of severity and chronicity.
The use of conventional sensors to evaluate hand movements requires the application of complicated and uncomfortable mechanical plugs. New technology has led to the development of sensor-bearing substrates flexible enough to be manufactured as garments.
Cutolo and Mancinelli are developing an upper limb rehabilitation system that, by combining robotics and virtual reality training with a comfortable sensing glove, will optimize motor restoration in patients with hemiparesis. "Creating textiles with embedded sensing elements by coating traditional fabrics with 'smart' materials has opened up new ways to implement the man-machine interface technology," they said.
The researchers added a sensing glove as an alternative input device. The system, an adjustable arm orthosis, reduces the effort required by the paretic arm to overcome gravity by passively counterbalancing the weight of the arm; the device augments feedback through virtual environments. Preliminary evidence supports the use of external support, such as that provided by the device, in motor function restoration in patients with hemiparesis.