Five Clues Implicating Natural Killer Cells in Human Autoimmunity
Discover several lines of evidence that NK cells play an important role in autoimmune disorders, in particular rheumatoid arthritis, lupus, and multiple sclerosis.
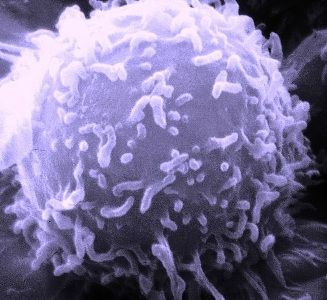
Natural Killer (NK) cells are innate lymphocytes that make up 5-15% of our peripheral blood mononuclear cells, and are also found in secondary lymphoid tissues. They play a crucial role in early host defense against viruses. By virtue of their ability to kill abnormal cells rapidly and to produce cytokines and chemokines, NK cells influence and shape adaptive immune responses and are positioned to play a role in regulating autoimmunity.
Several lines of evidence suggest that NK cells play an immunoregulatory role in T- and B-cell mediated human autoimmune disorders, in particular in rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and multiple sclerosis (MS).1
1. Many studies have reported that NKs in peripheral blood of patients with autoimmune diseases are decreased in number or impaired in cytotoxic function, but this may be misleading. These are correlative observations, based primarily on studies of peripheral blood samples, which cannot distinguish between true deficits and NK cell sequestration in target tissues. Furthermore, those rare patients who have complete deficiencies of NK cells show clinical courses dominated by overwhelming viral infections, not by autoimmune syndromes
2. Genetic association studies provide compelling evidence that NK cells contribute to the pathogenesis of numerous autoimmune disorders.2 The evidence arises from studies of killer immunoglobulin-like receptors (KIRs), polymorphic, germ-line-encoded receptors expressed on NK cells (and on a subset of T cells) that recognize human leukocyte antigens (HLA). KIR/HLA genotype combinations that favor activation of NK cells are often beneficial in protecting against infections.
For example, among individuals infected with HIV, the combination of KIR3DS1 and HLA-B Bw4-801 is associated with slower progression to AIDS and lower viral loads.3 However, these same activating KIR/HLA genotype combinations appear to predispose other individuals to autoimmune disorders, including Behcet’s disease, SLE, ankylosing spondylitis, and RA, as well as type I diabetes and MS.
Furthermore, the presence of activating KIRs or KIR/HLA genotypes in the context of decreased NK cell inhibition (e.g., absence of the corresponding inhibitory KIRs or the HLA ligands for the inhibitory KIRs) results in a lower activation threshold for NK cells (or potentially T cells), predisposing to autoimmune disorders including scleroderma and psoriatic arthritis.
3. Recent studies have implicated human NK cells in the pathogenesis of RA.4,5 RA patients have decreased circulating NK cells in their peripheral blood, with decreased cytotoxity on a per-cell basis, as do patients with juvenile idiopathic arthritis (JIA), with the most prominent deficits occurring in systemic JIA (sJIA) patients. Interestingly, however, NK cells comprise a significant fraction of the lymphocytes in the synovial fluid of swollen joints in RA patients, the majority of them being CD56bright NK cells, a subset that are more efficient cytokine and chemokine producers.6,7 Aberrant expression of NK-cell activation receptor ligands (e.g., MICA) in the inflamed synovium8 may augment CD56bright NK cell activation. Altogether, these phenomena may result in dysregulated production of proinflammatory cytokines, rather than in immunoregulation.
4. In MS, a temporal correlation between NK cell activity and periods of disease progression or remission supports the hypothesis that NK cells play an immunoregulatory role in disease pathology. For example, in a study of relapsing-remitting MS patients, depressed NK cell cytotoxicity preceded the appearance of MRI contrast-enhancing CNS lesions and the onset of clinical symptoms.9 Furthermore, CD56bright NK cells were substantially enriched in the CSF of MS patients as compared with paired blood samples, reminescent of the observations in the synovium of RA patients. Treatment of MS patients with daclizumab (a humanized anti IL-2Rα antibody) caused a significant expansion of CD56bright NK cells in the periphery, as well as a decrease in circulating CD4 T cells, and correlated with decreased MRI contrast-enhancing CNS lesions.105. Numeric deficits in peripheral NK cells, reported in multiple cohorts of SLE patients, correlate with clinical manifestations and overall disease activity. In addition to numeric deficits in peripheral NK cells, SLE patients and a subset of first degree relatives have depressed cytoxicity on a per-cell basis. A study in pediatric SLE patients demonstrated low numbers of peripheral NK cells and defective cytolysis (on a single cell level) at diagnosis or even prior to overt progression to SLE.11 (It should be noted that the majority of the human data on NK cells in SLE are correlative, and the role of NK cells in SLE is less well established than in RA and MS.)
All of these studies provide tantalizing but as yet incomplete evidence for the contributions of NK cells to the onset or progression of autoimmunity. A better understanding of their role may lead to novel therapeutic targets in these diseases
References:
REFERENCES
1. Fogel LA, Yokoyama WM, and French AR (2013) Natural killer cells in human autoimmune disorders.Arthritis Res Ther 15(4):216.
2. Kulkarni S, Martin MP, and Carrington M (2008) The Yin and Yang of HLA and KIR in human disease.Semin Immunol 20(6):343-352.
3. Alter G, Martin MP, Teigen N et al. (2007) Differential natural killer cell-mediated inhibition of HIV-1 replication based on distinct KIR/HLA subtypes.J Exp Med 204(12):3027-3036.
4. Ahern DJ and Brennan FM (2011) The role of Natural Killer cells in the pathogenesis of rheumatoid arthritis: major contributors or essential homeostatic modulators?Immunol Lett 136(2):115-121.
5. Conigliaro P, Scrivo R, Valesini G, and Perricone R (2011) Emerging role for NK cells in the pathogenesis of inflammatory arthropathies.Autoimmun Rev 10(10):577-581.
6. Dalbeth N and Callan MF (2002) A subset of natural killer cells is greatly expanded within inflamed joints.Arthritis Rheum 46(7):1763-1772.
7. Pridgeon C, Lennon GP, Pazmany L et al. (2003) Natural killer cells in the synovial fluid of rheumatoid arthritis patients exhibit a CD56bright,CD94bright,CD158negative phenotype.Rheumatology (Oxford) 42(7):870-878.
8. Groh V, Bruhl A, El-Gabalawy H, Nelson JL, & Spies T (2003) Stimulation of T cell autoreactivity by anomalous expression of NKG2D and its MIC ligands in rheumatoid arthritis.Proc Natl Acad Sci U S A 100(16):9452-9457.
9. Kastrukoff LF, Morgan NG, Zecchini D et al. (1998) A role for natural killer cells in the immunopathogenesis of multiple sclerosis. J Neuroimmunol 86(2):123-133.
10. Bielekova B, Howard T, Packer AN et al. (2009) Effect of anti-CD25 antibody daclizumab in the inhibition of inflammation and stabilization of disease progression in multiple sclerosis.Arch Neurol 66(4):483-489.
11. Yabuhara A, Yang FC, Nakazawa T, et al. (1996) A killing defect of natural killer cells as an underlying immunologic abnormality in childhood systemic lupus erythematosus.Journal of Rheumatology 23(1):171-177.