Acute Coronary Syndrome Rates Elevated in Patients With RA Receiving bDMARDs
Recent studies suggest that a gap in cardiovascular risk remains between patients with rheumatoid arthritis and the general population.
The 1-year, 2-year, and 5-year incidences of acute coronary syndrome (ACS) among patients with rheumatoid arthritis (RA) initiating biologic disease-modifying antirheumatic drugs (bDMARDs) were significantly higher when compared with the general population, according to a study published in BMJ Journals.1
“Efficacious treatment of RA inflammation should reduce cardiovascular disease (CVD) burden in RA, but while the absolute risks of CV events in the general population and in cohorts of patients with RA have declined substantially during the past decades, studies from recent years suggest that a gap in CV risk remains between these two populations,” investigators stated.
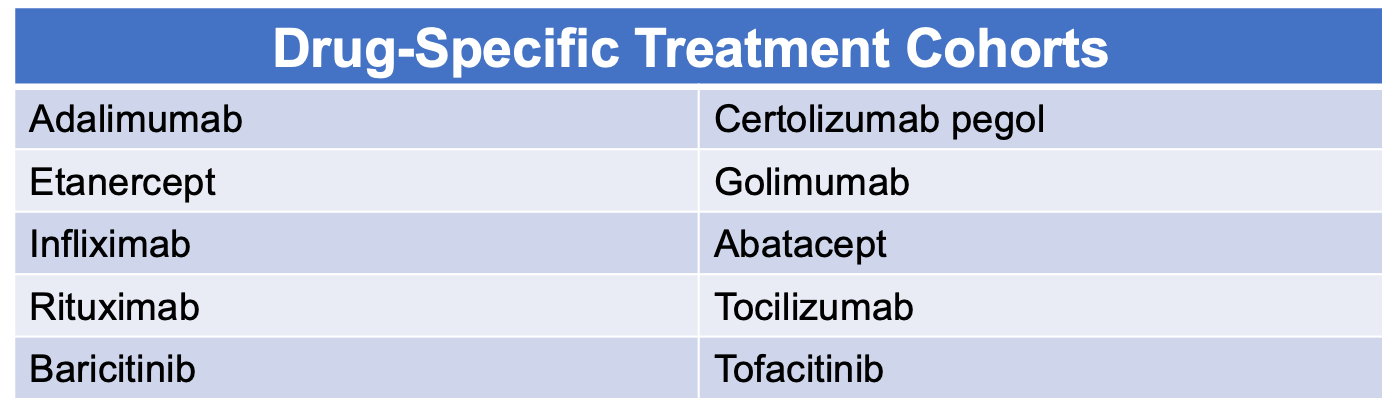
Patients with RA from Denmark (DANBIO), Norway (NOR-DMARD), Sweden (SRQ-ARTIS), and Finland (ROB-FIN) who started bDMARD between 2008 and 2017 were included in this observational cohort study. Incidence rates (IRs) of time to first ACS were calculated and compared across treatments (while accounting for ACS risk factors) as well as within the general population. The general population controls were matched (1:10 in Demark and 1:5 in Sweden) for sex, age, and area of residence.
Subgroups were further divided into age, history of cardiovascular disease, and the number of bDMARDs previously received. ACS was defined as hospitalization due to unstable angina, acute myocardial infarction (MI), subendocardial MI, or unspecific MI.
A total of 24,083 patients were included in the study (75% females, mean age 56 years). Etanercept was the most common treatment (27%), followed by adalimumab (14%), infliximab (13%), and rituximab (12%). During the 5-year follow-up period, 780 ACS events were reported.
Subgroup analysis showed that patients receiving abatacept had a higher likelihood of experiencing ACS. For patients with a history of CVD, HRs were similar across all treatment groups, with the exception of infliximab (1.49 [1.02-2.18]) during the follow-up period.
ACS rates in patients with RA were 80% higher than those in the general population cohort. Treatment-specific analyses showed a higher IR of ACS when compared with the control group.
While clinical characteristics and demographics were accounted for, other factors such as education level, sick leave, disability pension, and concomitant nonsteroidal anti-inflammatory drugs (NSAIDs) were unavailable. Further, ACS definition also varied between countries, which may have impacted the IRs.
The study was strengthened by the large number of patients and events included, which allowed investigators to conduct a comprehensive risk comparison. Algorithms defining ACS and other variables significantly reduced the risk of misclassification of ACS, outcomes, and covariates and ensured an independent assessment of ACS. Additionally, the inclusion of the general population cohort helped contextualize the results. Lastly, there was a fair evaluation of risks across treatment groups as all bDMARD options were assessed.
“As used in routine care, the risks of ACS in patients with RA starting a bDMARD vary little across individual drugs for short and intermediate terms,” investigators concluded. “Our results suggest that in RA treated with bDMARDs, the bDMARD used does not seem to matter for the risk of ACS.”
Reference:
Delcoigne B, Ljung L, Provan SA, et al. Short-term, intermediate-term and long-term risks of acute coronary syndrome in cohorts of patients with RA starting biologic DMARDs: results from four Nordic countries [published online ahead of print, 2022 Mar 22]. Ann Rheum Dis. 2022;annrheumdis-2021-221996. doi:10.1136/annrheumdis-2021-221996