Cannabis Significantly Improves Quality of Life in Women with Treatment-Resistant Fibromyalgia
As cannabis use continues to rise worldwide, investigators question its role in treating fibromyalgia, a common pain syndrome that affects women twice as much as men.
Treatment with cannabis resulted in a short-term beneficial effect on quality of life, regarding its influence on pain, sleep, psychological, and physical domains, in women with treatment-resistant fibromyalgia, according to a study published in Pain Practice.1
“As the worldwide use of cannabis rises, investigators question its role in treating fibromyalgia as one of the most common pain syndromes nowadays,” investigators explained. “Throughout history, different cultures used cannabis to treat pain. Modern medicine found the endocannabinoid system's role in the pathophysiology of neuropathic pain. Previous studies showed that cannabis is efficacious in promoting sleep, deepening, and lengthening the sleep cycle. Other advantages of cannabis treatment include good pain relief without significant side effects.”
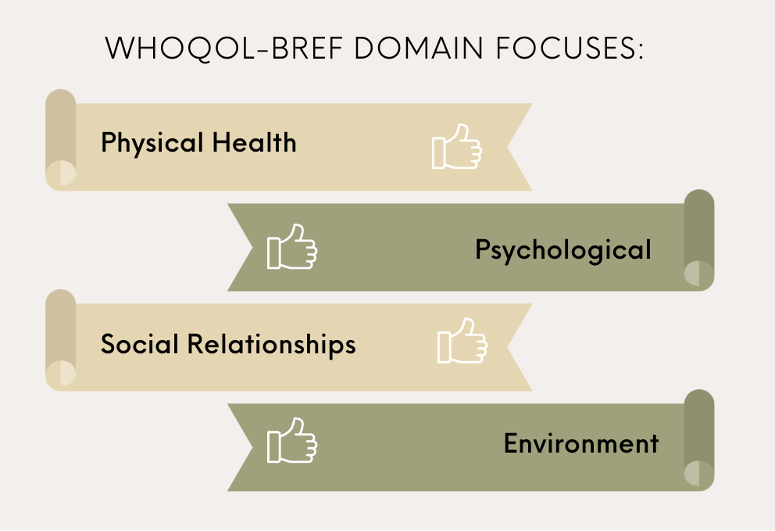
The prospective cohort study used the World Health Organization Quality of Life Bref questionnaire (WhoQoL-bref), a simple, validated tool that evaluates patient-reported QoL, to better understand the impact of treatment with cannabis in 30 women aged 18-70 years with treatment-resistant fibromyalgia, defined as having exhausted pharmacological fibromyalgia treatment. The WhoQoL-bref focused on 4 domains: psychological, physical health, social relationships, and environment. The questionnaire was filled prior to cannabis initiation and at the 1-month follow-up. Patients were able to choose their route of administration, such as smoking, vaporizing, or ingestion. Patients were excluded if they were younger than 18 or older than 70, had cognitive impairment, were pregnant, or were already using cannabis treatment.
The mean age of participants was 46 years and were experiencing pain and discomfort (3.77 ± 1.3), a dependence on medication (3.07 ± 1.74), poor QoL (1.47 ± 0.63), reduced activities of daily living (1.47 ± 0.82), and poor general health (1.47 ± 0.78) at baseline prior to intervention. Environmental factors, including access to health and social care, financial resources, transport, and physical environment, were high, indicating fibromyalgia-related morbidity as opposed to environmental restraints.
At the follow-up, treatment was linked to improvements in general quality of life (1.97 out of a 5-point score, p< 0.01), activities of daily living (2.13, p< 0.01), psychological domain (1.3, p< 0.01), general health (1.83, p< 0.01), physical health (1.5, p< 0.01), and reductions in pain and discomfort (p< 0.01) and pain and fatigue (1.57, p< 0.01). Improvements were also shown in the sub-domain fields within the psychological domain, including self-esteem (1.1 points, p< 0.01), recreation and leisure (0.97 points, p<0.01), memory and concentration (1.4 points, p< 0.01), positive feelings (1.07 points, p< 0.01), and sex(1.37 points, p< 0.01). Home environment (p= 0.31) and financial resources (p = 0.07) were not impacted by cannabis treatment.
The relatively small sample size, short follow-up period, and lack of a comparison group limited the study. Additionally, biases may include the pre- and post-study design and the possibility of selection bias. However, improvements in QoL following treatment were statistically significant. Future research should examine the mental effects of cannabis as well as a time- or dose-dependent waning of treatment.
“Further studies are still indicated to understand this potential and its long-term impact,” investigators concluded. “Future epidemiologic studies should examine other confounders such as body mass index (BMI), anxiety, depression, personality disorders or traits, chronic medical issues, and various regular medications.”
Reference:
Hershkovich O, Hayun Y, Oscar N, Shtein A, Lotan R. The role of cannabis in treatment-resistant fibromyalgia women [published online ahead of print, 2022 Nov 4]. Pain Pract. 2022;10.1111/papr.13179. doi:10.1111/papr.13179