Diagnosis and management of cervical spine injuries in athletes
Cervical spine injuries are common in athletes, particularly those engaged in contact sports.
Cervical spine injuries are common in athletes, particularly those engaged in contact sports. American football and diving are the sports most often associated with these injuries.1 Although most cervical spine injuries have a benign natural history with limited morbidity, catastrophic spine injuries, along with head injuries, account for 70% of the traumatic deaths and 20% of the permanent disability related to sports.2 The rate of quadriplegia for high school and college football players in the United States is 0.50 and 0.82 per 100,000, respectively.3 Participation in tackle football has increased 24% from 1998 to 2007, placing more young athletes at risk for cervical spine injury.4
Sports-related cervical spine injuries can affect muscles, ligaments, intervertebral disks, vertebrae, and the neural structures they protect (Table 1). Neck injuries deserve special attention for their potential to affect the spinal cord, potentially resulting in death or crippling permanent disability. The possibility of a catastrophic neurological injury in the setting of an unstable spine fracture necessitates meticulous on-field evaluation. Timely patient evaluation and prevention of further injury are the physician's key objectives. An accurate initial clinical assessment is needed to determine whether a player needs further medical evaluation and care or can return to the game safely.
In this article, we survey the spectrum of cervical spine disorders seen in athletes, ranging from muscle strains to spinal cord injury. We emphasize well-organized initial care and identification of conditions that require immediate hospital-level care.
INITIAL ON-FIELD EVALUATION
Preparation is the first step in effective management of on-field injuries. The staff requires education about the nature of cervical spine injuries and the steps in evaluating an injured player so that at the moment of injury the response team executes a plan learned through rehearsal. A spine board, a hard cervical collar, and cardiopulmonary resuscitation equipment must be available. A trained and equipped staff is then ready to take the field to assess a player.5
During on-field evaluation, the clinician must suspect a cervical spinal cord injury until it is proved otherwise. On reaching the player, the clinician must control him or her and his position because he may have lost consciousness and, on awakening, routinely will attempt to move. The physician needs to calmly talk to the player and explain what he and his team are doing as they examine him.
First line of action
A player with suspected spine injury is not moved without immobilization unless absolutely necessary to maintain the ABCs-Airway, Breathing, and Circulation. The basic life support survey of ABCs is the first line of action for the response team. A player who must be moved is placed in the supine position with the team holding his head and neck in a neutral position, and then the standard ABC protocol is followed.
Airway assessment begins by removing the mouth guard, if present, and then maintaining an unobstructed airway.6,7 The jaw thrust technique is the safest approach to opening the airway of an athlete with suspected spinal cord injury. This is performed by placing your fingers behind the angles of the jaw and then pushing the jaw forward or by hooking your fingers under the jaw and pulling forward. The lips are separated to allow breathing through the mouth as well as the nose. These maneuvers are performed without rotating the head.
Moving the jaw forward lifts the tongue and the epiglottis away from the back of the throat and opens the airway. If the jaw thrust does not open the airway, then the head can be tilted backward with care to avoid overextension of the neck. For an athlete who is not wearing a helmet, a cervical collar must be placed on the athlete if there is any evidence of bone or spinal cord involvement.1
For players wearing helmets, the facemask should be removed to facilitate airway access. This can be a challenge, because the design of helmets and rusting of bolts from exposure can make one tool more or less effective than another.
Again, staff preparation is crucial. The response team must familiarize themselves with the facemask design that their players use. Most facemasks are secured to the helmet with loop straps. A screwdriver can be used to remove the loop straps, but this may not work if the bolts and screws have rusted.
Masks secured to the helmet with loop straps traditionally have been cut with a "trainer's angel," although this device has proved less effective with the more recent design of loop straps. A gardening tool, the anvil pruner, has proved effective as the ideal device for facemask removal, according to a report from the Inter-Association Task Force for Appropriate Care of the Spine-Injured Athlete.7 Whatever the tool used, practicing to determine the ideal implement for removal of the kind of facemasks that the team uses is recommended.
Assess breathing
Breathing is assessed by looking, listening, and feeling for air flow. Because the diaphragm receives innervation from C3, C4, and C5, injury at or above these levels can result in paralysis of the diaphragm. A nonbreathing player should receive artificial respiration with a bag-valve mask or other available device. Circulation rarely is impaired if there has not been a cardiac injury.7
Injuries to the cervical spine and the head often occur together, and even when both are not present in an athlete, there is overlap in the clinical presentation of these injuries. Consciousness is evaluated by assessing orientation, ability to follow commands, and eye opening. The patient's behavior can be scored formally with the Glasgow Coma Scale, which correlates with prognosis for brain injuries.5,7 When regaining consciousness, the athlete may be agitated and may require additional assistance to maintain spine precautions.
If the player is wearing a helmet and shoulder pads, they will maintain the cervical spine in a neutral position when the player is supine. Both shoulder pads and helmet must be removed at the same time to retain the spine's neutral alignment. The circumstances in which the helmet and shoulder pads are removed on the field are rare. They include the inability to access the airway or remove the facemask promptly, a loose-fitting helmet that the head moves around within, and the inability to fasten the helmet to the spine board during pretransportation immobilization. Ideally, the player is transported while wearing the helmet and shoulder pads for controlled removal at a medical facility.7
Neurological examination is needed
Once the ABCs have been assessed and stabilized, a complete neurological examination is needed. If there is no evidence of a neurological injury, palpate along the spinous processes and facets, which are just lateral to the paraspinal muscles at this level. If they have point tenderness, they will need to be placed on a spine board and sent for further imaging.
If the athlete has no pain or tenderness of the cervical spine, he can be allowed to gently rotate his head (active range of motion) to determine whether he feels pain with movement. If the player is pain-free with neck movement, he can sit up. If the clinician has any doubt and suspects that a player has a cervical spine injury, the next step is to transfer him to a spine board.
Immobilization required
Transportation of the patient with a suspected cervical spine injury requires immobilization on a rigid spine board. Most clinicians are familiar with the logroll technique of transferring a patient to a spine board. The large size of many athletes combined with the bulkiness of their equipment renders the familiar logroll technique an imperfect method of maintaining spine alignment while transferring patients.
Recent study has demonstrated that the 6-plus-person lift probably is the best technique to move an injured player.8 One responder stabilizes the neck by placing hands palm up under the player's shoulders (or shoulder pads) with the player's head resting on forearms. Then a responder is positioned at each side of the player's chest and pelvis, and 1 to each leg. Each responder slides his arms solidly under the player. The leader then gives the command to lift, and simultaneously the responders lift the player 4 to 6 inches off the ground and a spine board is slid underneath, starting at the foot end. A command is then given to lower the player in coordinated fashion.7
If the helmet has been removed, a hard cervical collar can be applied. Otherwise, the helmet is strapped or taped to the spine board with towels or a cervical vacuum splint is used to support the cervical spine. Then the torso, pelvis, and legs are strapped to the board.
Proportions differ in children
Children have an increased size of head relative to torso compared with adults, a difference in proportions that has led researchers to question whether younger children with suspected spine injury should have their helmet and shoulder pads removed as a unit. The increased size of head places a supine child's cervical spine into relative flexion when on a flat surface. For children 6 years and younger, a spine board with a recessed well for the head is used to maintain the spine in neutral when the child is supine.
A recent study of children aged 8 to 14 years lying supine on a flat surface showed that cervical spine alignment is identical with helmet and shoulder pads and without. A significant difference in curvature occurs when shoulder pads are worn alone. For the 8-to 14-year-old group, shoulder pads and helmet are to be treated as a unit and removed together to maintain the spine's sagittal alignment, just as is done with older athletes.9
For athletes transported to a medical facility for further care of a suspected cervical spine injury, permanent immobilization measures are instituted, then the helmet and shoulder pads may be removed. To remove the helmet, the chin strap is unfastened and then the cheek pads are removed. Next, the athlete's head is supported at the occiput by one person while another spreads the earflaps and pulls the helmet off in a direction perfectly in line with the cervical spine.1,6,10
Under difficult circumstances, bolt cutters may be used to cut off the helmet. Spinal alignment is maintained as the blade is inserted into the front midline of the helmet, always keeping the blade's tip in view. Hurrying is rarely needed. We advise proceeding slowly and cautiously because this will be done in a controlled tertiary environment in which assistance for emergent airway management or vascular decline is nearby.
CERVICAL SPINE ANATOMY
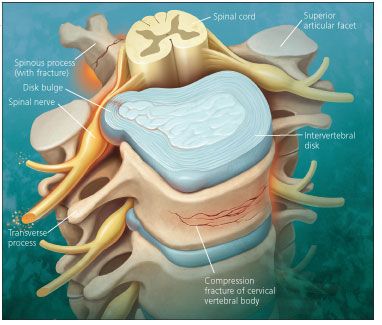
The spine supports the head and helps protect neural structures (Figure). It also provides the neck with extensive mobility. In the occiput (C0)-C1-C2 complex, the major stabilization for the C0-C1 (occipitocervical) articulation is provided by the bony conformity between the occipital condyles and the articulating lateral masses of the atlas. The articulation of the odontoid process to the atlas is retained by the transverse ligament; rotation is limited by the alar and apical ligaments. The posterior longitudinal ligament plays a crucial role in cervical spine stability. High-energy trauma is a major cause of instability in the C0-C1 region and resulting injuries.
COMMON NECK INJURIES IN ATHLETESCervical sprain or strainDefinition: A sprain is a stretching injury to a ligament. At its most extreme, the ligament is torn, possibly resulting in instability of the affected joint. A strain is a stretching or tearing of muscle fibers.11
Diagnosis: Muscle strains in the neck typically result when individual fibers tear during a strong eccentric contraction elicited by direct traumatic force to the head or neck. Sprains of the facet joint capsular ligaments can occur with forced flexion and are more likely to occur in children because of their ligamentous laxity and less robust musculature.
These injuries usually occur in contact sports and at the extremes of motion, such as hyperflexion, hyperextension, and excessive rotation. The typical characteristics are cervical pain and restrictions in range of motion.
Cervical x-ray films are necessary to evaluate for instability. Anteroposterior (AP), lateral, and open mouth views are obtained for all cervical injuries to evaluate for fracture and subluxation.
At most centers, CT scanning for patients with spine injures is done after basic x-ray films. If asymmetry is present between the spinous processes on the spine lateral film, a ligamentous injury must be considered and strict cervical spine precautions maintained. Note that this may not be demonstrated on the CT scan.
Results of radiographic evaluation and the neurological examination are normal in patients with a sprain or muscle strain. MRI is the gold standard for identification of ligamentous injury.11
Management: As with all cervical spine injuries, first the neck is immobilized until resolution of muscle spasm allows for full flexion and extension radiographs to rule out dynamic instability, which may be a period of 7 to 10 days.11 Initial management is symptomatic, with NSAIDs, analgesics, and cryotherapy.
Use of an ice pack for 10 minutes or ice massage usually is helpful for acute strains. For ice massage, a plastic foam cup filled with water is placed in the freezer. Once it has frozen, the top of the cup is peeled down to expose the ice. This is placed directly onto the skin over the injury site and moved in small circles about the area. The cold sensation changes to a prickly sensation, followed by numbness. About 5 minutes after numbness occurs, the cryotherapy can be stopped. Once initial symptoms subside, moist heat, gentle stretching, and light isometric exercises can be started until there is full, spasm-free range of motion in the neck.12
Muscular torticollisDiagnosis: Torticollis, a twisted or bent position of the neck, most often occurs in athletes as a result of unilateral neck muscle spasm producing a characteristic side bent and rotated posture of the head. This condition is seen in racket sports, where there is frequent explosive neck rotation, and in activities that require prolonged positioning of the neck, such as marksmanship. It also may be seen with C1-C2 issues, but this is exceedingly rare and would be identified during the cervical spine radiological evaluation.
Management: Initial treatment modalities include NSAIDs and analgesics, plus ice and a soft collar. A home cryotherapy session starts with the athlete supine with the neck in a comfortable position and an ice pack applied to the tense musculature as identified by the physician. Then an assistant passively rotates the athlete's neck every 10 minutes until there is discomfort. This new position is then maintained, and then the ice pack is replaced. Repeating this procedure, first in 1 direction of rotation and then the opposite, usually restores normal range of motion.
Intervertebral disk injuriesDiagnosis: Cervical disk herniations typically occur when axial loading and hyperflexion result in trauma (eg, in divers, wrestlers, and football linebackers). The athlete typically presents with neck pain that can radiate down the arm if the disk contacts a nerve root. Nerve root involvement also can cause tingling, numbness, weakness, and reduced or absent reflexes.
A massive disk herniation can compress the spinal cord, causing an acute anterior cervical spinal cord syndrome. This syndrome is characterized by immediate paralysis of all 4 limbs accompanied by loss of pain and temperature below the level of the lesion. However, there is preservation of light touch sensation.12,13
Plain x-ray films are the first images obtained when looking for disk-space narrowing. MRI is ideal for assessing disks and nerve roots, but if the mechanism of injury raises suspicion of a fracture, a CT scan should be performed first, because identification and surgical correction of instability is of higher priority than management of radiculopathy.
Management: This is initially conservative, with the use of NSAIDs, analgesics, and medications specific for neuropathic pain if there is radicular discomfort. Physical therapy with foraminal opening maneuvers, neural stretching, and cervical strengthening exercises are initiated to accomplish the dual goals of pain relief and restoration of function. Traction is a useful modality for patients who have radicular symptoms because it decompresses the cervical spine, slightly widening the foramen to relieve pressure from nerve roots. Home traction units can be prescribed. When the player does not improve with conservative care, a surgical evaluation can be obtained.
Compression fractureDiagnosis: Compression fractures are seen much more frequently in thoracic and lumbar regions but occasionally are found in the cervical region, typically between the C4 and C7 levels (see Figure in Journal). The diagnosis is made with plain x-ray films or CT.
Management: After these fractures are detected, plain x-ray films often are followed with a CT scan to determine the extent of fracture involvement, because an unstable burst fracture may be present. If there is less than 25% anterior compression, conservative care with analgesics and cervical orthosis is appropriate. Greater than 50% anterior compression on plain x-ray films is an indication of possible instability because the posterior longitudinal ligament often is affected. If there is any concern about fracture stability, a surgical consultation is mandatory.14
Spinous process fracturesDiagnosis: Spinous process fractures (see Figure in Journal) can result from several mechanisms. The most common is avulsion of the spinous process tip through intense trapezius and rhomboid contraction or extreme cervical flexion or extension causing ligament strain that avulses bone. Fracture from direct bony trauma is uncommon.
Diagnosis of these fractures is made with plain radiographs. Flexion-extension views are obtained at a time when the patient tolerates range of motion, which may be several weeks after the injury.11
Management: A spinous process fracture in isolation is not a cause for concern. Treatment is supportive with a cervical collar for pain relief and immobilization until flexion-extension views are obtained.11 When the spinous process is nontender, range of motion exercises are initiated and physical therapy is started. Return to play is considered for stable healed compression or spinous fracture if it is without neurological deficit and range of motion is full and pain-free.14
Stinger/burnerDefinition: This is an injury to the nerves coming off the spinal cord, most often a nerve root but sometimes the brachial plexus. The injury derives its name from the characteristic immediate onset of "stinging" or "burning" neuropathic pain. Mechanisms of stinger injury include traction to the brachial plexus from ipsilateral shoulder depression and contralateral neck flexion and compression of the cervical roots or brachial plexus from ipsilateral lateral flexion and hyperextension.15,16
Diagnosis: The patient often complains of burning pain and may have weakness. A complete cervical spine and neurological examination is performed. Spinal tenderness suggests fracture, and involvement of more than 1 limb suggests spinal cord injury. Both require immediate immobilization and further evaluation.17
The diagnosis can be confirmed by performing the Spurling test. This maneuver involves cervical extension, lateral bending, and axial compression; reproduction of pain is considered an abnormal test result. Electrodiagnostic studies (electromyography and nerve conduction studies) help localize the site of damage and assess the patient's prognosis.
Symptoms must be present for at least 3 weeks to maximize the diagnostic yield. To rule out bony involvement, plain radiographs of the cervical spine should be obtained. MRI can readily demonstrate neuroforaminal stenosis and disk abnormalities, including herniation and degeneration, but is less sensitive for fracture detection.15
Management: Treatment of patients with stingers is supportive. Symptom control initially is pursued with medications and a sling is used to reduce traction on nerve roots if symptoms worsen when the arm is in a dependent position. Physical therapy is started rapidly to prevent further loss of function.
The first goal is to restore pain-free mobility with gentle stretching. Next, strengthening is achieved with use of concentric and eccentric loading at various speeds and in supine, prone, and side-lying positions.15 During the rehabilitative process, positions that compromise the cervical nerves, such as excessive flexion, are avoided and posture principles emphasized. Finally, the athlete strengthens the scapular stabilizers, thoracic extensor musculature, and upper limbs.
For prevention, a review of proper tackling positions with the head up and face on the ball can be reviewed. In addition, football players can add high neck rolls that limit lateral bending and extension.17 The athlete can return to play when full cervical range of motion is regained without pain and there is resolution of any neurological deficit. If the symptoms are associated with a disk herniation, this is managed as a radiculopathy described previously. If the player has had 3 stinger injuries in a season or a single stinger with symptoms lasting more than a day, return to play is somewhat contraindicated.17
Spinal cord injuriesDefinition: Transient spinal cord injury, termed "cervical cord neurapraxia," falls into 3 grades based on duration: grade 1, less than 15 minutes; grade 2, 15 minutes to 24 hours; and grade 3, longer than 24 hours.18 Permanent spinal cord injuries are categorized based on the American Spinal Injury Association impairment scale, a discussion of which is beyond the scope of this article, which will focus on transient quadriplegia.
Diagnosis: Axial load to a flexed or extended spine can cause transient quadriplegia, a syndrome of bilateral deficits of motor and/or sensory function.19 The patient is immobilized and treated as though he had an unstable fracture until proved otherwise.
Once a more serious injury is ruled out and after symptoms resolve, the delicate issue of return to play must be dealt with. A player ready to return to play is one who has full resolution of symptoms and a history of only 1 quadriplegic episode. He has full range of motion, normal spine alignment, and no instability. In addition, MRI or CT myelography demonstrates functional reserve space around the spinal cord.20
Even with the above criteria being met, a thorough discussion with the athlete and, with permission, the family and coach, ensures that the physician is presenting a consistent message. It also ensures that the potential risks of reinjury are addressed and deflects any confounding pressures on the athlete from the physician as his advocate.
ADDITIONAL RETURN-TO-PLAY GUIDELINES
Many sets of guidelines have been established for other spinal conditions not covered in this article. An example is shown in Table 2. Do not become complacent with this population. They generally are motivated and recover well, but they may underrepresent issues so they can return to sports activity. Remaining consistent in your approach and evaluating the patient fully allows you to provide appropriate care for this population.
CONCLUSION
Cervical spine complaints are frequent in sports. Most often the injury is a matter of temporary discomfort for the athlete, who soon returns to play. The potential for a catastrophic cervical injury presents itself in each sporting encounter. This challenges the physician to respond to each injury as though it is the most severe.
By suspecting an unstable spine fracture, the response team is prepared to maximize the chances of survival and functional recovery in the rare instance of true spinal cord injury. Preparation takes the form of education and an action plan.
All injuries are assessed with AP, lateral, and odontoid views of the cervical spine. If there is no fracture and the player is able to actively flex and extend, dynamic views are obtained to evaluate for instability. If the player has too much pain to fully flex and extend, then a hard cervical collar is worn until pain subsides to allow these views. Physical therapy is used to help the patient regain function.
References:
References1. Warren WL Jr, Bailes JE. On the field evaluation of athletic neck injury. Clin Sports Med. 1998;17:99-110.
2. Proctor MR, Cantu RC. Head and neck injuries in young athletes. Clin Sports Med. 2000;19:693-715.
3. Boden BP, Tacchetti RL, Cantu RC, et al. Catastrophic cervical spine injuries in high school and college football players. Am J Sports Med. 2006;34:1223-1232.
4. National Sporting Goods Association. 2007 Youth Participation in Selected Sports With Comparisons to 1998. http://www.nsga.org. Accessed January 20, 2009.
5. Ghiselli G, Schaadt G, McAllister DR. On-the-field evaluation of an athlete with a head or neck injury. Clin Sports Med. 2003;22:445-465.
6. Vegso JJ, Torg, JS. Field evaluation and management of cervical spine injuries. In: Torg JS, ed. Athletic Injuries to the Head, Neck, and Face. 2nd ed. St Louis: Mosby; 1991:426-437.
7. National Athletic Trainers' Association. Prehospital Care of the Spine-Injured Athlete: A Document From the Inter-Association Task Force for Appropriate Care of the Spine-Injured Athlete. 2001. http://www.nata.org/statements/consensus/NATAPreHospital.pdf. Accessed January 20, 2009.
8. Del Rossi G, Horodyski MH, Conrad BP, et al. The 6-plus-person lift transfer technique compared with other methods of spine boarding. J Athl Train. 2008;43:6-13.
9. Treme G, Diduch DR, Hart J, et al. Cervical spine alignment in the youth football athlete: recommendations for emergency transportation. Am J Sports Med. 2008;36:1582-1586.
10. Torg JS. Management guidelines for athletic injuries to the cervical spine. Clin Sports Med. 1987;6:53-60.
11. Zmurko MG, Tannoury TY, Tannoury CA, Anderson DG. Cervical sprains, disc herniations, minor fractures, and other cervical injuries in the athlete. Clin Sports Med. 2003;22:513-521.
12. Torg JS, Genarelli TA. Intracranial and cervical spine injuries. In: Garrett W Jr, Speer KP, Kirkendall DT, eds. Principles and Practice of Orthopedic Sports Medicine. Philadelphia: Lippincott Williams & Wilkins; 2000:153-182.
13. Schneider RC, Kennedy JC. The treatment of the athlete with neck, cervical spine, and spinal cord trauma. In: Schneider RC, Kennedy JC, Plant M, eds. Sports Injuries: Mechanisms, Prevention, and Treatment. Baltimore: Williams & Wilkins; 1985:676-698.
14. Boden BP, Jarvis CG. Spinal injuries in sports. Neurol Clin. 2008;26:63-78; viii.
15. Weinstein SM. Assessment and rehabilitation of the athlete with a "stinger": a model for the management of noncatastrophic athletic cervical spine injury. Clin Sports Med. 1998;17:127-135.
16. Kuhlman GS, McKeag DB. The "burner": a common nerve injury in contact sports. Am Fam Physician. 1999;60:2035-2040, 2042.
17. Weinberg J, Rokito S, Silber JS. Etiology, treatment, and prevention of athletic "stingers." Clin Sports Med. 2003;22:493-500, viii.
18. Castro FP Jr. Stingers, cervical cord neurapraxia, and stenosis. Clin Sports Med. 2003;22:483-492.
19. Fagan K. Transient quadriplegia and return-to-play criteria. Clin Sports Med. 2004;23:409-419.
20. Anderson P, Steinmetz M, Eck J. Head and neck injuries in athletes. In: Spivak JM, Connolly PJ, eds. Orthopaedic Knowledge Update: Spine 3. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2006:259-270.