Differentiating low and high ankle sprains
Differentiation between low and high ankle sprains iscritical to delivering appropriate care.The classic mechanism for a lowankle sprain is inversion and plantar flexion. A history of ankle ligamentinjury predisposes to recurring sprains. The ankle anterior drawertest may be used to evaluate ligamentous instability. Plain radiographsof the foot and ankle may be indicated in a patient who has an acuteankle injury. Clinicians often use the Ottawa ankle rules to determinethe need for radiographs. In the acute phase, the goals of treatment areto alleviate pain, reduce swelling, and protect the ankle from furtherinjury. NSAIDs and rehabilitation are important components of management.Primary prevention may be possible with strengthening andbalance programs. (J Musculoskel Med. 2008;25:438-443)
ABSTRACT: Differentiation between low and high ankle sprains is critical to delivering appropriate care. The classic mechanism for a low ankle sprain is inversion and plantar flexion. A history of ankle ligament injury predisposes to recurring sprains. The ankle anterior drawer test may be used to evaluate ligamentous instability. Plain radiographs of the foot and ankle may be indicated in a patient who has an acute ankle injury. Clinicians often use the Ottawa ankle rules to determine the need for radiographs. In the acute phase, the goals of treatment are to alleviate pain, reduce swelling, and protect the ankle from further injury. NSAIDs and rehabilitation are important components of management. Primary prevention may be possible with strengthening and balance programs. (J Musculoskel Med. 2008;25:438-443)
Ankle sprains are the most common musculoskeletal injury in athletes, accounting for 10% to 30% of sports injuries.1 Differentiation between low and high (syndesmotic) sprains is critical to delivering appropriate care to patients who sustain either injury.
An understanding of the anatomy and biomechanics of the ligaments that provide stability to the ankle and distal tibiofibular joint, as well as the risk factors for ankle sprains, is essential to performing a competent clinical evaluation. In most cases, applying this knowledge during the physical examination allows for an accurate diagnosis.
This 2-part article defines the salient points of clinical evaluation of ankle sprains to differentiate between low and high sprains and, as a result, provide patients with the most appropriate treatment. In this first part, we focus on low ankle sprains. The second part, to appear in a later issue of this journal, will discuss diagnosis and management of high ankle sprains.
BACKGROUND
Acute ankle injuries are especially common in persons who participate in basketball, racquet sports, gymnastics, volleyball, and soccer. 1-3 Athletes who compete at higher levels of play are at increased risk for ankle sprains4; they are the most common injury in college athletes, according to the National Collegiate Athletic Association Injury Surveillance Survey results, accounting for 15% of reported injuries. 5 Ligamentous injuries to the ankle are the most common injury regardless of the sport or exposure type (game or practice).1,5
The incidence of re-injury in athletes with ankle sprains is significantly higher than the incidence of first-time ankle sprains.6 Disability resulting from ankle sprains may be severe; 40% of patients experience dysfunction for as long as 6 months after the injury. In a Marchi and associates7 study, 23% of ankle sprains resulted in permanent sequelae over 12 years.
The cost of treating patients with ankle sprains is staggering. In 2003 alone, the direct medical cost of managing ankle sprains was more than $1 billion, according to US Consumer Products Safety Commission estimates.8
ANATOMY AND BIOMECHANICS
Both osseous congruity and ligaments confer stability to the ankle joint. Osseous congruity exists between the tibiotalar and distal tibiofibular joints.
The ligaments on the lateral side of the ankle consist of the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament (PTFL) (Figure 1). The relationship between the positions of the talus and the longitudinal tibial axis determines the function of the ankle ligaments. The ATFL is perpendicular and the CFL is parallel to the longitudinal axis of the tibia with the ankle in neutral dorsiflexion. In this position, the CFL resists inversion stress and varus tilt of the talus. With dorsiflexion, the CFL experiences more strain. With plantar flexion, internal rotation, and inversion, strain increases in the ATFL.
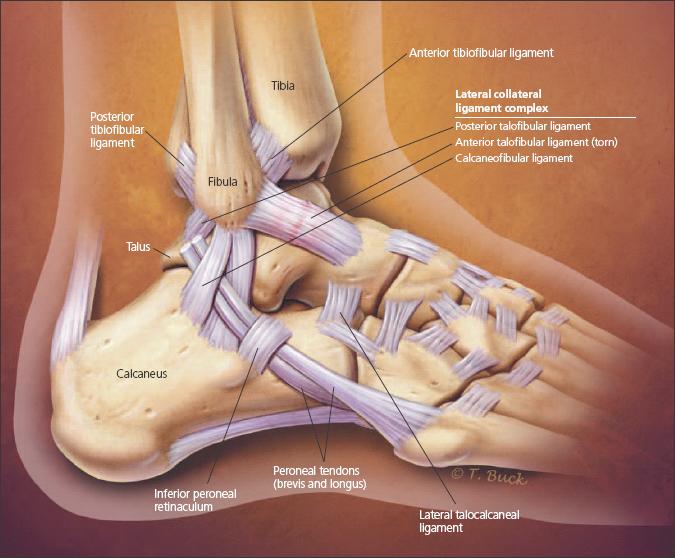
Figure 1 -
The lateral anatomy of the lower ankle is shown in this drawing. Both osseous congruity and ligaments confer stability to the ankle joint. The ligaments on the lateral side consist of the anterior talofibular ligament, calcaneofibular ligament, and posterior talofibular ligament. The relationship between the positions of the talus and the longitudinal tibial axis determines the function of the ankle ligaments. Plantar flexion is the position in which a lateral ankle ligament injury most often occurs.
Plantar flexion is the position in which a lateral ankle ligament injury most often occurs. In this position, the ATFL is parallel and the CFL is perpendicular to the longitudinal axis of the tibia. The ATFL is at risk for injury in this position because it provides resistance against inversion stress. Most low lateral ankle sprains occur with plantar flexion and inversion; the ATFL is the most frequently injured ligament with this mechanism.9 High arches, increased foot width, and limited dorsiflexion appear to have a higher risk of inversion ankle
injuries.10-12
Overall, the ATFL and CFL work in a reciprocal relationship to provide lateral stability to the ankle joint. Tearing of the ankle ligaments occurs as increasing load is applied to them. The ATFL usually fails first and the deep deltoid last.13
On the medial side, ankle ligaments include the superficial deltoid (tibionavicular ligament, tibiospring ligament, tibiocalcaneal ligament, and superficial tibiotalar ligament) and the deep deltoid (deep anterior tibiotalar ligament and deep posterior tibiotalar ligament). Isolated injury to the deltoid ligament is rare. Most deltoid ruptures occur concomitantly with ankle fractures. Instability may result if the deep portion of the ligament is torn.14
CLINICAL ASSESSMENT
History
The classic mechanism for a low ankle sprain is inversion and plantar flexion. Patients often describe "rolling" their ankle inward. A patient who describes an eversion mechanism may have an injury to the deltoid ligament.
Typically, patients with lateral ankle ligament sprains describe swelling, difficulty with ambulation, and pain over the lateral aspect of the ankle. Complaints of numbness or paresthesia, inability to bear weight, or coldness in the foot warrant more immediate evaluation. The clinician must have a high suspicion for compartment syndrome when these signs are present or when pain is out of proportion.15 A patient who can bear weight immediately after an injury is more likely to have a ligament injury than a fracture.
In most patients who present with this history and physical examination, the diagnosis is a low ankle sprain. However, high ankle sprains and osteochondral injuries of the talus also must be considered as isolated or concomitant sources of pain after the initial injury.
A history of ankle ligament injury predisposes to recurring sprains. If a patient reports having a previous sprain, the physician should inquire about the type of rehabilitation performed after the previous injury. If the type and duration of rehabilitation did not allow for soft tissue healing, recovering range of motion, improving strength, and re-establishing proprioception, the patient will not recover from the initial injury and will be at risk for chronic morbidity with respect to ankle function.
As a cause of ankle pain, instability may be described as mechanical or functional. Mechanical instability has been described as ankle range of motion that exceeds the physiological limitations. This mechanical instability is assessed using the anterior drawer test and the talar tilt test. More that 10 mm of anterior translation on 1 side and more than 3 mm of side-to-side difference are parameters commonly used in the diagnosis of mechanical instability. However, functional instability is a subjective feeling of the ankle "giving way" during physical activity or during everyday routines after a sprain. In this setting, mobility occurs beyond voluntary control, but physiological range of motion is not necessarily exceeded.
Physical examination
Careful inspection of an injured ankle helps identify gross deformity and swelling. Active and passive range of motion should be assessed with plantar flexion, dorsiflexion, eversion, and inversion. Palpation for tenderness should include the full length of the fibula, both malleoli, the medial and lateral ankle ligaments, the ATFL, the talus, the base of the fifth metatarsal, the navicular, the peroneal tendons, the talar dome, and the anterior joint line.
Ankle laxity tests aid in the assessment of ligament injuries and are useful in grading sprains. A comparison always should be made between the injured and noninjured ankles.
Ankles may be graded as follows:
• Grade 1: no disruption of the ankle ligaments.
• Grade 2: a partial ligament tear is involved.
• Grade 3: sprain is equivalent to a complete ligament tear.
The ankle anterior drawer test may be used to evaluate ligamentous instability. The test is performed with the ankle in slight plantar flexion (Figure 2). The examiner stabilizes the lower leg and pulls forward on the calcaneus to assess anterior translation of the talus with respect to the distal tibia. The presence of laxity suggests disruption of the ATFL. Again, comparison needs to be made with the noninjured ankle to differentiate physiological laxity from pathologic instability caused by the injury.
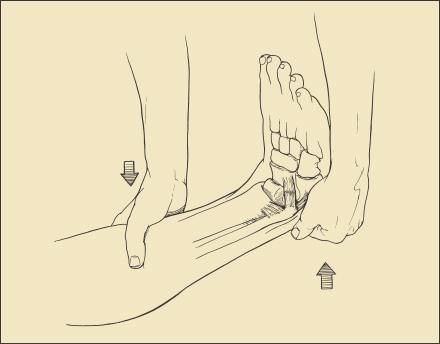
Figure 2
- Ligamentous instability may be assessed with the ankle anterior drawer test. The test is performed with the ankle in slight plantar flexion. The examiner stabilizes the lower leg and pulls forward on the calcaneus to assess anterior motion.The presence of laxity suggests disruption of the anterior talofibular ligament.
The talar tilt test checks for medial and lateral movement of the calcaneus and the talus relative to the tibia and fibula. Abnormal laxity with a varus stress indicates damage to the ATFL and CFL. Comparison with the uninjured ankle often helps differentiate physiological and injury-related laxity from instability. With a grade 2 injury, mild laxity is present with the anterior drawer test, but there is a firm end point. Patients with a grade 3 injury have laxity without a definite end point.
van Dijk and colleagues16 compared physical examination of the ankle with arthrography; delayed physical examination (5 days after injury) was 96% sensitive and 84% specific in detecting lateral ankle ligament disruption. Delayed physical examination was more accurate than an examination conducted in the first 48 hours because swelling and pain interfere with the ability to detect abnormal laxity accurately during this period.
Imaging
Plain radiographs of the foot and ankle may be indicated in a patient who has an acute ankle injury. Clinicians often use the Ottawa ankle rules to determine the need for radiographs.17 These rules recommend ankle radiographs for patients with bony tenderness over the posterior edge or tip of either malleolus or the inability to bear weight (for 4 steps) at the time of injury and at the time of assessment. Foot radiographs are indicated with midfoot pain, as well as the inability to bear weight or tenderness over the navicular or fifth metatarsal base.18
Multiple studies have been conducted to assess the validity of the Ottawa rules. A recent meta-analysis reported that when the Ottawa rules are applied to ankle injuries, the sensitivity for detecting fractures is between 96.4% and 99.6% and the specificity is between 26.3% and 47.9%.19
PRINCIPLES OF TREATMENT
Nonoperative
In the acute phase of injury after an ankle sprain, the goals of treatment are to alleviate pain, reduce swelling, and protect the ankle from further injury. The preferred management of ankle sprains in the acute phase is RICE (Rest, Ice, Compression, Elevation). Cryotherapy for acute musculoskeletal injuries helps control the acute inflammatory response to injury. Although there are no large randomized controlled trials that demonstrate a statistically significant benefit to using ice for ankle sprains, some evidence from smaller studies suggests that cryotherapy reduces swelling and decreases recovery time.20
NSAIDs are another important component of nonoperative management. Placebo-controlled studies have shown that NSAIDs help relieve pain and inflammation after acute ankle sprains.21-23 In one study, diclofenac was superior to ibuprofen and piroxicam in controlling pain and inflammation.24 Celecoxib, a cyclooxygenase 2 (COX-2) inhibitor, is at least as effective as nonspecific COX inhibitors, such as ibuprofen and diclofenac, in allowing patients to return to activities and decreasing pain. However, whether the significantly higher cost of COX-2 inhibitors is justified in the management of ankle sprains is unclear.22,25-27
Rehabilitation is an essential component of low ankle sprain management. Functional therapy consists of using an external support for the ankle with early, controlled mobilization. With functional treatment, patients initially use RICE therapy immediately after injury. Subsequently, they progress through a program of physical therapy, which starts with range of motion exercises and advances to strengthening exercises. In the final phase of treatment, patients work on sport-specific and proprioception training exercises. Recent comprehensive literature reviews have shown that this strategy is preferable to providing treatment by completely immobilizing the joint with a cast or boot in the acute phase of injury.28-32 Patients who undergo functional treatment return to sports and work sooner than patients who do not.
What type of splint is optimal in the acute phase after a low ankle sprain is not well established. An ankle stirrup or semi-rigid brace allows for quicker return to activities and improves function more than elastic bandages.30-32 For grade 1 and 2 ankle sprains, combining an air-stirrup brace with an elastic wrap results in faster return of function than using either method of support alone. Lace-up ankle braces may provide an advantage over semi-rigid braces by helping alleviate swelling.31
Additional modalities, such as ultrasonography, often are used in the management of low ankle sprains, but their efficacy is unproved.33 In fact, a recent literature review showed that in placebo-controlled studies, ultrasonography does not decrease disability, pain, or swelling or improve range of motion.33
Operative
Surgical management of acute ankle sprains is rare.34 Surgery usually is reserved for patients who do not respond to conservative measures and who have residual, symptomatic ankle instability.This situation is most common after severe injury and in cases of chronic injury. The techniques include direct repair of torn ligaments and reconstruction procedures that use grafts to replace deficient ligaments.
PREVENTION
A study of basketball players revealed that athletes are nearly 5 times more likely to sustain an ankle sprain if they have a history of a previous sprain.6 Most trials examining how to help athletes avoid ankle injuries focus on secondary prevention-how to prevent ankle sprain recurrence.
However, some evidence indicates that primary prevention of ankle sprains may be possible with strengthening and balance programs. Poor balance, as measured by the ability to maintain a single leg stance and postural sway, is a risk factor for sustaining an ankle sprain.35-37 Physical therapy programs that emphasize proprioception and balance have been studied extensively in recent years. Efforts to improve these factors significantly reduce the risk of ankle sprains.38-43 However, stretching programs have not decreased the risk of ankle sprains.11,38
The cost-effectiveness of instituting proprioception programs for athletes who have no previous history of sprains is unclear. However, providing this type of training for a person who has a history of ankle sprains clearly is justifiable.44
Many athletes who participate in high-risk sports wear external ankle supports to prevent ankle sprains. Athletes who sustain ankle sprains while wearing an external support appear to have the same severity of injury as those who participate in sports without braces.38 In one small study, external orthoses did not appear to prevent recurring sprains in athletes who had sustained more than 3 sprains in their careers.42
Recently, the cost-effectiveness of taping has been questioned; data support the use of external braces to prevent ankle sprains.38,45-46 In fact, the average cost of taping each ankle during an entire sports season is greater than the cost of commercially available braces.45
Barrett and associates47 conducted a prospective randomized trial to look at whether shoe type affects the risk of ankle sprains. Athletes were randomized to wear high-top basketball shoes, high-tops with inflatable air chambers, or low-top basketball shoes. No significant differences were seen in ankle sprain rates between the groups, suggesting that shoe type does not affect an athlete's risk of ankle ligament injury.
Practice Points
• The lateral ligament complex, specifically the anterior talofibular ligament, is most frequently injured in ankle sprains.
• The deep deltoid ligament is the primary ligament stabilizing the ankle joint.
• Rehabilitation is an essential component of managing stable low and high ankle sprains.
References:
References
- 1. Fong DT, Hong Y, Chan LK, et al. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37:73-94.
- 2. Garrick JG, Requa RK. The epidemiology of foot and ankle injuries in sports. Clin Sports Med. 1988;7:29-36.
- 3. Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28:112-116.
- 4. Beynnon BD, Vacek PM, Murphy D, et al. First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med. 2005;33:1485-1491.
- 5. Hootman JM, Dick R, Agel T. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42:311-319.
- 6. McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35:103-108.
- 7. Marchi AG, Di Bello D, Messi G, Gazzola G. Permanent sequelae in sports injuries: a population based study. Arch Dis Child. 1999;81:324-328.
- 8. Verhagen EA, van Meechelen W, de Vente W. The effect of preventive measures on the incidence of ankle sprains. Clin J Sport Med. 2000;10:291-296.
- 9. Fallat L, Grimm DJ, Saracco JA. Sprained ankle syndrome: prevalence and analysis of 639 acute injuries. J Foot Ankle Surg. 1998;37:280-285.
- 10. Morrison KE, Kaminski TW. Foot characteristics in association with inversion ankle injury. J Athl Train. 2007;42:135-142.
- 11. Pope R, Herbert R, Kirwan J. Effects of ankle dorsiflexion range and pre-exercise calf muscle stretching on injury risk in Army recruits. Aust J Physiother. 1998;44:165-172.
- 12. Tabrizi P, McIntyre WM, Quesnel MB, Howard AW. Limited dorsiflexion predisposes to injuries of the ankle in children.
J Bone Joint Surg. 2000;82B:1103-1106.
- 13. Attarian DE, McCrackin HJ, DeVito DP, et al. Biomechanical characteristics of human ankle ligaments. Foot Ankle. 1985;6:54-58.
- 14. Earll M, Wayne J, Brodrick C, et al. Contribution of the deltoid ligament to ankle joint contact characteristics. Foot Ankle Int. 1996;17:317-324.
- 15. Creighton RA, Kinder J, Bach BR Jr. Compartment syndrome following recurrent ankle inversion injury. Orthopedics. 2005;28:703-705.
- 16. van Dijk CN, Lim LS, Bossuyt PM, Marti RK. Physical xamination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg. 1996;78B:958-962.
- 17. Markert RJ, Walley ME, Guttman TG, Mehta R. A pooled analysis of the Ottawa ankle rules used on adults in the ED. Am J Emerg Med. 1998;16:564-567.
- 18. Stiell IG, Greenberg GH, McKnight RD, et al. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Ann Emerg Med. 1992;21:384-390.
- 19. Bachmann LM, Kolb E, Koller MT, et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ. 2003;326:417.
- 20. Sloan JP, Hain R, Pownall R. Clinical benefits of early cold therapy in accident and emergency following ankle sprain. Arch Emerg Med. 1989;6:1-6.
- 21. Bahamonde LA, Saavedra H. Comparison of the analgesic and anti-inflammatory effects of diclofenac potassium versus piroxicam versus placebo in ankle sprain patients. J Int Med Res. 1990;18:104-111.
- 22. Ekman EF, Fiechtner JJ, Levy S, Fort JG. Efficacy of celecoxib versus ibuprofen in the treatment of acute pain: a multicenter, double-blind, randomized controlled trial in acute ankle sprain. Am J Orthop. 2002;31:445-451.
- 23. Moran M. An observer-blind comparison of diclofenac potassium, piroxicam and placebo in the treatment of ankle sprains. Curr Med Res Opin. 1990;12:268-274.
- 24. Moran M. Double-blind comparison of diclofenac potassium, ibuprofen and placebo in the treatment of ankle sprains. J Int Med Res. 1991;19:121-130.
- 25. Gomez Cerezo J, Lubomirov Hristov R, Carcas Sansuan A, Vazquez Rodriguez J. Outcome trials of COX-2 selective inhibitors: global safety evaluation does not promise benefits. Eur J Clin Pharmacol. 2003;59:169-175.
- 26. Nadarajah A, Abrahan L, Lau FL, et al. Efficacy and tolerability of celecoxib compared with diclofenac slow release in the treatment of acute ankle sprain in an Asian population. Singapore Med J. 2006;47:534-542.
- 27. Petrella RJ, Petrella MJ, Cogliano A. Periarticular hyaluronic acid in acute ankle sprain. Clin J Sport Med. 2007;17:251-257.
- 28. Ardèvol J, BolÃbar I, Belda V, Argilaga S. Treatment of complete rupture of the lateral ligaments of the ankle: a randomized clinical trial comparing cast immobilization with functional treatment. Knee Surg Sports Traumatol Arthrosc. 2002;10:371-377.
- 29. Kerkhoffs GM, Rowe BH, Assendelft WJ, et al. Immobilization and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002;(3):CD003762.
- 30. Kerkhoffs GM, Rowe BH, Assendelft WJ, et al. Immobilization for acute ankle sprain. A systematic review. Arch Orthop Trauma Surg. 2001;121:462-471.
- 31. Kerkhoffs GM, Stuijs PA, Marti RK, et al. Different functional treatment strategies for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002;(3):CD002938.
- 32. Boyce SH, Quigley MA, Campbell S. Management of ankle sprains: a randomised controlled trial of the treatment of inversion injuries using an elastic support bandage or an Aircast ankle brace. Br J Sports Med. 2005;39:91-96.
- 33. Van Der Windt DA, Van Der Heijden GJ, Van Den Berg SG, et al. Ultrasound therapy for acute ankle sprains. Cochrane Database Syst Rev. 2000;(2):CD001250.
- 34. Kerkhoffs GM, Handoll HH, de Bie R, et al. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2007;(2):CD000380.
- 35. de Noronha M, Refshauge KM, Herbert RD, et al. Do voluntary strength, proprioception, range of motion, or postural sway predict occurrence of lateral ankle sprain? Br J Sports Med. 2006;40:824-828.
- 36. McGuine TA, Greene JJ, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10:239-244.
- 37. Trojian TH, McKeag DB. Single leg balance test to identify risk of ankle sprains. Br J Sports Med. 2006;40:610-613.
- 38. Handoll HH, Rowe BH, Quinn KM, de Bie R. Interventions for preventing ankle ligament injuries. Cochrane Database Syst Rev. 2001;(3):CD000018.
- 39. Holme E, Magnusson SP, Becher K, et al. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104-109.
- 40. McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2006;34:1103-1111.
- 41. Mohammadi F. Comparison of 3 preventive methods to reduce the recurrence of ankle inversion sprains in male soccer players. Am J Sports Med. 2007;35:922-926.
- 42. Stasinopoulos D. Comparison of three preventive methods in order to reduce the incidence of ankle inversion sprains among female volleyball players. Br J Sports Med. 2004;38:182-185.
- 43. Verhagen E, van der Beek A, Twisk J, et al. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32:1385-1393.
- 44. Verhagen EA, van Tulder M, van der Beek AJ, et al. An economic evaluation of a proprioceptive balance board training program for the prevention of ankle sprains in volleyball. Br J Sports Med. 2005;39:111-115.
- 45. Mickel TJ, Bottoni CR, Tsuji G, et al. Prophylactic bracing versus taping for the prevention of ankle sprains in high school athletes: a prospective, randomized trial. J Foot Ankle Surg. 2006;45:360-365.
- 46. Jerosch J, Thorwesten L, Bork H, Bischof M. Is prophylactic bracing of the ankle cost effective? Orthopaedics. 1996;19:405-414.
- 47. Barrett JR, Tanji JL, Drake C, et al. High- versus low-top shoes for the prevention of ankle sprains in basketball players: a prospective randomized study. Am J Sports Med. 1993;21:582-585.