Differentiating osteopoikilosis from osteoblastic metastases
ABSTRACT: Osteopoikilosis is a rare, benign osteosclerotic dysplasiathat predominantly involves the appendicular skeleton. Radiographicfindings are diagnostic, and the disease often is discovered incidentallyon x-ray films. The importance of recognizing osteopoikilosis liesin differentiating it from osteoblastic metastases. The cause is unclear.Patients typically are asymptomatic. Diagnostic findings include theappearance of numerous small,well-defined, spheroid sclerotic foci.Because evidence suggests an association with skeletal and dermatologicalchanges, evaluation for coexisting pathological conditions maybe warranted. The differential diagnosis for a patient who has radiographiccharacteristics similar to those of osteopoikilosis includes osteoblasticmetastases, mastocytosis, tuberous sclerosis, melorheostosis,and osteopathia striata. (J Musculoskel Med. 2008;25:387-389)
ABSTRACT: Osteopoikilosis is a rare, benign osteosclerotic dysplasia that predominantly involves the appendicular skeleton. Radiographic findings are diagnostic, and the disease often is discovered incidentally on x-ray films. The importance of recognizing osteopoikilosis lies in differentiating it from osteoblastic metastases. The cause is unclear. Patients typically are asymptomatic. Diagnostic findings include the appearance of numerous small, well-defined, spheroid sclerotic foci. Because evidence suggests an association with skeletal and dermatological changes, evaluation for coexisting pathological conditions may be warranted. The differential diagnosis for a patient who has radiographic characteristics similar to those of osteopoikilosis includes osteoblastic metastases, mastocytosis, tuberous sclerosis, melorheostosis, and osteopathia striata. (J Musculoskel Med. 2008;25:387-389)
Osteopoikilosis, which literally means "spotted bones," is a rare, benign osteosclerotic dysplasia that was first described in the early 20th century.1-5 The disease, seen in men and women of all ages, predominantly involves the appendicular skeleton. It occurs most often in bones of the hands and feet, although lesions are seen scattered around larger joints.3,5,6 The pathogenesis is unknown, although mutations in the LEMD3 gene may be the cause.7,8
Radiographic findings are diagnostic, and the disease often is discovered incidentally on x-ray films. Medical evaluation may be important, however, because there may be coexisting developmental or pathological conditions.9
The importance of recognizing osteopoikilosis lies in differentiating it from osteoblastic metastases.2 Gaining a better understanding of the disease may alleviate both patient and physician anxiety. In addition, having knowledge of this radiographic entity may minimize unnecessary testing and medical costs. In this article, we describe the epidemiology of osteopoikilosis, the history and physical examination, radiographic characteristics, the histology, associations with skeletal and dermatological changes, and the differential diagnosis.
Incidence, epidemiology, causes
The incidence of osteopoikilosis is estimated at 1 in 50,000; the disease is seen in up to 6 per 100,000 radiographs.3,10 This benign skeletal dysplasia has no age or sex predilection. Osteopoikilosis usually is discovered in patients aged 15 to 60 years, but fetal and geriatric cases have been reported. The cause of osteopoikilosis is unclear. The disease probably is transmitted in an autosomal dominant fashion, although sporadic forms are documented.5,9,11-13 The pathogenesis is thought to involve perturbation of collagen regulation or failure to form trabeculae along the lines of stress.5,10 Evidence suggests a relationship with other osteosclerotic skeletal disorders, especially osteopathia striata and melorheostosis.4,13
History and physical examination
Patients with osteopoikilosis typically are asymptomatic, although 15% to 20% report mild articular pain and joint effusion.5,11,14 Overt external physical findings otherwise are absent. Whether the mild symptoms are related to osteopoikilosis or to the inciting injury that led to the indication for radiography is uncertain.5,9,11 Because the condition is thought to be without symptoms, discovery by radiographic examination most often is incidental.
Radiographic characteristics
Findings diagnostic of osteopoikilosis include the appearance of numerous small, well-defined, spheroid sclerotic foci-usually ranging from 2 to 10 mm-clustered in periarticular regions (Figure).3,5,9 These well-delineated opacities most often are seen in the small bones of the hands (carpus) and feet (tarsus).5
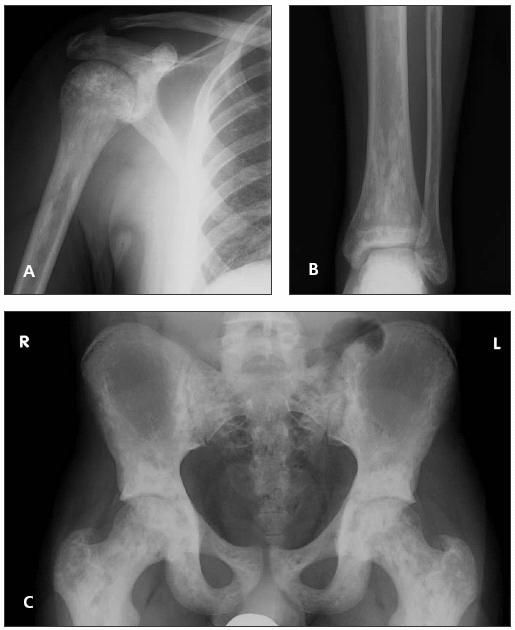
Figure –
Radiographic findings diagnostic of osteopoikilosis include the appearance of numerous small, well-defined, spheroid sclerotic foci clustered in periarticular regions in the shoulder (A), ankle (B), and pelvis (C).
In the epiphyses of tubular bones, the foci rarely contact the subchondral bone plate. The metaphyseal lesions may be located eccentrically, abutting the endosteal cortical surface.4
The chief distribution of lesions in the pelvis is found about the acetabulum; this distribution appears to be related to the orientation of trabecular bone.15 The long axes of the sclerotic foci parallel the long axes of the bones involved.3
The scapula may show involvement around the glenoid. The skull, mandible, clavicles, sternum, ribs, and spine usually are not affected.4
On serial radiographs, the radio-opaque areas may increase or decrease in size, remain the same, or even disappear.4,13 Once growth plate closure occurs, however, the lesions usually do not change in size or appearance.3
Histology
The histology of the lesions consists of thickened trabeculae of lamellar osseous tissue that contains haversian systems lying within the cancellous structure; they probably represent foci of bone that did not become cancellous during growth and differentiation.2,10 The condensation of cancellous bone in osteopoikilosis consists of a peripheral area of trabeculae in which osteocytes are scant and there are no osteoblasts or osteoclasts (both are present in the central core of irregular trabeculae). The precise origin of these abnormal areas remains debatable, but they appear to represent foci of deranged differentiation in cancellous bone.9
Associations
Osteopoikilosis is a benign condition, but considerable evidence suggests an association with skeletal and dermatological changes.5,13 Therefore, evaluation for coexisting pathological conditions may be warranted.
In an association known as Buschke-Ollendorf syndrome (osteopoikilosis and dermatofibrosis lenticularis disseminata),3,5,10 there is a tendency toward keloid formation. In addition, pea-sized fibrous skin papules accompany the bone lesions in 25% of cases; these papules usually are widely distributed over the patient's trunk and extremities.16
Osteopoikilosis also has been associated with scleroderma, syndactyly, dwarfism, endocrine abnormalities, cleft palate, dystocia, spinal stenosis, and tuberous sclerosis.4,5,17 Another associated condition is mixed sclerosing bone dysplasia, a rare triad of benign bone disorders-osteopoikilosis, osteopathia striata, and melorheostosis-that occur in concert.3,17
Differential diagnosis
The differential diagnosis for a patient who has radiographic characteristics similar to those of osteopoikilosis includes osteoblastic metastases, mastocytosis, tuberous sclerosis, melorheostosis, and osteopathia striata.3,5 However, these other conditions have additional distinguishing physical findings on clinical examination. The discriminating radiographic features should help support the diagnosis of osteopoikilosis.
Radionuclide bone scanning may play a critical role in differentiating osteopoikilosis from primary or metastatic bone disease. In osteopoikilosis, the bone scan result usually is somewhat normal. Although an abnormal result does not rule out osteopoikilosis, bone scanning has been used to differentiate the process from metastatic bone disease.2,5,11,14 The bone scan of a patient with metastatic disease usually reveals increased uptake at the lesion (hot spot). If multiple sites are involved, an asymmetrical distribution may be expected throughout the skeleton.2,4,9,11,12
Mastocytosis and tuberous sclerosis have bone lesions that are symmetrical, uniform, and well-defined with a predilection for metaphyseal and epiphyseal areas; all are less striking than those in osteopoikilosis.4 In melorheostosis, there is thickening along the endosteal and periosteal bone that has been described as having a "candle dripping" appearance, which helps differentiate the pathology from osteopoikilosis.3 Osteopathia striata (Voorhoeve disease) is a benign disorder characterized by longitudinal dense striations in affected bones that is thought to be a variant of osteopoikilosis.3,4,15 This condition often is asymptomatic and, like osteopoikilosis, is discovered by accident. 3 Another bone disorder, Paget disease, may be distinguished from osteopoikilosis with radionuclide scanning; it also has radiographic differences.
References:
References
- 1. Benli IT, Akalin S, Boysan E, et al. Epidemiological, clinical and radiological aspects of osteopoikilosis. J Bone Joint Surg. 1992;74B:504-506.
- 2. Tong EC, Samii M, Tchang F. Bone imaging as an aid for the diagnosis of osteopoikilosis. Clin Nucl Med. 1988;13:816-819.
- 3. McLennan MK. Radiology rounds: osteopoikilosis. Can Fam Physician. 1999;45:2315, 2318-2320.
- 4. Niwayama G. Enostosis, hyperstosis, and periostitis. In: Resnick D, ed. Diagnosis of Bone and Joint Disorders. Philadelphia: WB Saunders; 1988:4084-4088.
- 5. Borman P, Ozoran K, Aydog S, Coçskun S. Osteopoikilosis: report of a clinical case and review of literature. Joint Bone Spine. 2002;69:230-233.
- 6. Gunal I, Seber S, Basaran N, et al. Dacryocystitis associated with osteopoikilosis. Clin Genet. 1993;44:211-213.
- 7. Hellemans J, Preobrazhenska O, Willaert A, et al. Lossof-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet. 2004;36:1213-1218.
- 8. Mumm S, Wenkert D, Zhang X, et al. Deactivating germline mutations in LEMD3 cause osteopoikilosis and Buschke-Ollendorff syndrome, but not sporadic melorheostosis. J Bone Miner Res. 2007;22:243-250.
- 9. Havitçioglu H, Günal I, Göçen S. Synovial chondromatosis associated with osteopoikilosis-a case report. Acta Orthop Scand. 1998;69:649-650.
- 10. Drouin CA, Grenon H. The association of Buschke-Ollendorf syndrome and nail-patella syndrome. J Am Acad Dermatol. 2002;46:621-625.
- 11. Mungovan JA, Tung GA, Lambiase RE, et al. Tc-99m MDP uptake in osteopoikilosis. Clin Nucl Med. 1994;19:6-8.
- 12. Whyte MP, Murphy WA, Siegel BA. 99mTc-pyrophosphate bone imaging in osteopoikilosis, osteopathia striata, and melorheostosis. Radiology. 1978;127:439-443.
- 13. Chigira M, Kato K, Mashio K, Shinozaki T. Symmetry of bone lesions in osteopoikilosis: report of 4 cases. Acta Orthop Scand. 1991;62:495-496.
- 14. Wadhwa SS, Mansberg R. Abnormal bone scan in osteopoikilosis. Clin Nucl Med. 1999;24:71-72.
- 15. Lagier R, Mbakop A, Bigler A. Osteopoikilosis: a radiological and pathological study. Skeletal Radiol. 1984;11:161-168.
- 16. Albertini JG, Maroon M, Tyler WB. Widespread pea-sized papules and gooseflesh plaques in a 44-year-old woman. Arch Dermatol. 2000;136:1055-1060.
- 17. Butkus CE, Michels VV, Lindor NM, Cooney WP 3rd. Melorheostosis in a patient with familial osteopoikilosis. Am J Med Genet. 1997;72:43-46.