Injection of the anserine bursa and iliotibial tract
ABSTRACT: Inflammation of the anserine bursa occurs frequently inathletes who have tight hamstrings, obese patients, patients who haveknee joint pathology, and those who experience direct trauma to thearea. Iliotibial band syndrome results from inflammation of the iliotibialtendon and the bursa. For both injections, the patient may beinjected while lying supine with the leg extended. During anserinebursa injection, the lidocaine and corticosteroid should flow withoutresistance, although some pressure is required. An inability to depressthe syringe plunger requires repositioning of the needle to avoid injectioninto the medial collateral ligament or pes anserinus tendons.(J Musculoskel Med. 2008;25:340-341)
ABSTRACT: Inflammation of the anserine bursa occurs frequently in athletes who have tight hamstrings, obese patients, patients who have knee joint pathology, and those who experience direct trauma to the area. Iliotibial band syndrome results from inflammation of the iliotibial tendon and the bursa. For both injections, the patient may be injected while lying supine with the leg extended. During anserine bursa injection, the lidocaine and corticosteroid should flow without resistance, although some pressure is required. An inability to depress the syringe plunger requires repositioning of the needle to avoid injection into the medial collateral ligament or pes anserinus tendons. (J Musculoskel Med. 2008;25:340-341)
Pes anserine bursitis is a common finding in patients who present with anteromedial knee pain. The pes anserine ("goose foot") bursa is located between the medial collateral ligament (MCL) and the medial hamstring tendons along the proximal tibia. The medial hamstrings-sartorius, gracilis, and semitendinosus-merge into a common tibial insertional attachment, the pes anserinus, which forms the roof of the pes anserine bursa. This bursa reduces friction where motion occurs between the medial hamstrings and the MCL. Inflammation of the bursa occurs frequently in athletes who have tight hamstrings; in persons who have continual rotary and valgus stress, as seen in obese patients; in patients who have knee joint pathology, which causes hamstrings to spasm; and in persons who experience direct trauma to the area.
In iliotibial band syndrome (ITBS), patients generally report pain at the lateral aspect of the knee. The ITB is connective tissue that originates from the anterior superior iliac spine region and runs down the lateral portion of the thigh; it inserts on the lateral tibial condyle (LTC) and the distal portion of the femur. ITBS results from inflammation of the iliotibial tendon and the bursa, which lies underneath as it rubs against the lateral femoral condyle (LFC). Because repeated knee flexion and extension can provoke ITB irritation, ITBS is common in longdistance runners.
This article is the ninth in a 12- part series on the most frequently injected joints and bursae. Here we focus on the anserine bursa and iliotibial tract.
Suggested supplies
• 3-mL syringe with 1 mL of 1% lidocaine for both anserine bursa and ITB injections.
• 3-mL syringe with 15 mg of prednisone equivalents (we prefer 10 to 20 mg of a nonfluorinated corticosteroid, eg,methylprednisolone, for the anserine bursa and the ITB) admixed with 0.5 to 1 mL of 1% lidocaine.
• 1- or 1.5-inch 25-gauge needle for both injections.
• Alcohol wipes,povidone-iodine, or chlorhexidine for sterilization.
• Local anesthetic: ethyl chloride topical spray (optional).
• Needle cap or ballpoint pen to mark the site of insertion.
• Nonsterile gloves.
• Gauze pads and bandage.
Surface anatomy
Anserine bursa: The anserine bursa is localized at the level of the tibial tubercle 1.5 to 2 inches below the medial tibiofemoral joint line. The area of maximum point tenderness is marked.
Iliotibial band: Palpate for point tenderness over the LFC or LTC, especially when flexing or extending the knee, as the ITB slides across the LFC. Pain also may be elicited with active abduction and passive adduction of the leg.
Patient position
For both injections, the patient may be injected while lying supine with the leg extended.The pes anserine bursa also may be injected with the patient seated and the knee flexed.
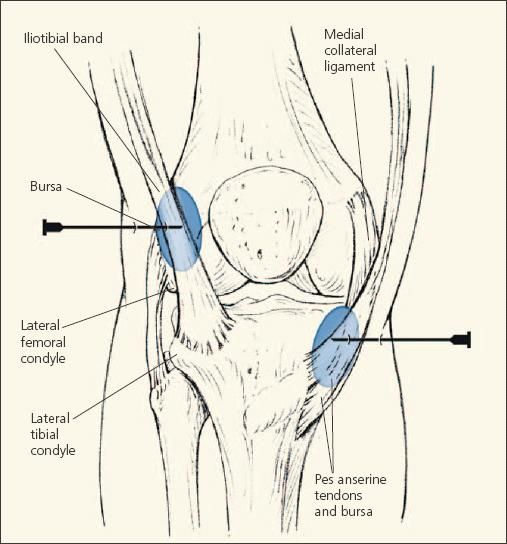
Figure –
Patients who present with anteromedial knee pain often have pes anserine bursitis. To inject the anserine bursa, advance the needle perpendicular to the skin with a cephalad tilt toward the medial tibial plateau. Patients with iliotibial band syndrome generally report pain at the lateral aspect of the knee. For injection, the needle is advanced perpendicular to the skin just above the lateral femoral condyle at the point of maximum tenderness with a cephalad tilt.
Procedure
Anserine bursa: After sterilization and injection of local anesthetic to the periosteum, a 25-gauge needle is advanced perpendicular to the skin with a cephalad tilt toward the medial tibial plateau (Figure).The needle is advanced to the tibial periosteum and then withdrawn ¹⁄? inch to avoid injection into the MCL.Once the needle is located between the MCL and pes anserine tendon at the bursal space, the anesthetic and corticosteroid contents are infused.
Iliotibial band: After sterilization and injection of local anesthetic to the periosteum, a 25-gauge needle is advanced perpendicular to the skin just above the LFC at the point of maximum tenderness with a cephalad tilt. The needle is advanced to the femoral periosteum and then withdrawn ¹⁄? inch, and the bursal region is infiltrated with anesthetic and corticosteroid.
Pearls
During anserine bursa injection, the lidocaine and corticosteroid should flow without resistance, although some pressure is required to inject through a small 25-gauge needle. An inability to depress the syringe plunger requires repositioning of the needle by a few millimeters to avoid injection into the MCL or pes anserinus tendons.
Therapeutic agents mentioned in this article:
Methylprednisolone
Prednisone