Making Important Clinical Decisions in Osteoporosis Management
Involving patients in decision making may help improve the quality of care.

ABSTRACT: Osteoporosis is a common disease that is associated with a high risk of fractures, which result in increased morbidity, mortality, and health care costs. Although good clinical tools are available to make a diagnosis and there are many options for prevention and treatment, the condition remains underdiagnosed and undertreated. When medication is prescribed, patients often do not continue to take it or do not take it correctly. Clinical decisions in the management of osteoporosis include selection of patients for bone density testing, evaluation for factors that contribute to low bone mass, identification of patients likely to benefit from treatment, advising specific nonpharmacological and pharmacological therapy, and monitoring treatment. Involving patients in decision making may help improve the quality of care. (J Musculoskel Med. 2008;25:11-19)
Osteoporosis is a common disease characterized by low bone mineral density (BMD) and poor bone quality that reduces bone strength and increases the risk of fragility (low-trauma) fractures.1 The lifetime risk of fracture at age 50 years is about 53% in women and 21% in men.2 In 2005, an estimated 2 million-plus osteoporosis-related fractures occurred in the United States; direct health care costs reached nearly $17 billion.3 Vertebral fractures and hip fractures are associated with increased morbidity and mortality.4
Despite the availability of good clinical tools for identifying patients at risk for fracture, osteoporosis is underdiagnosed in clinical practice. This is the case even in patients who have already sustained a fragility fracture and are at very high risk for future fracture.
Osteoporosis also is undertreated, even though many prevention and treatment options have become available. Even when patients are treated, many do not take medication correctly or for a sufficient duration to reduce fracture risk. Of those patients who start therapy, the persistence rate at 1 year typically is reported at 50% or lower.5 Poor persistence is associated with poor clinical outcomes (fractures) and increased health care costs.
The vast majority of patients with osteoporosis can be treated effectively. To reduce the burden of osteoporotic fractures on individual patients and on society, physicians must become knowledgeable about the latest diagnosis and management strategies.
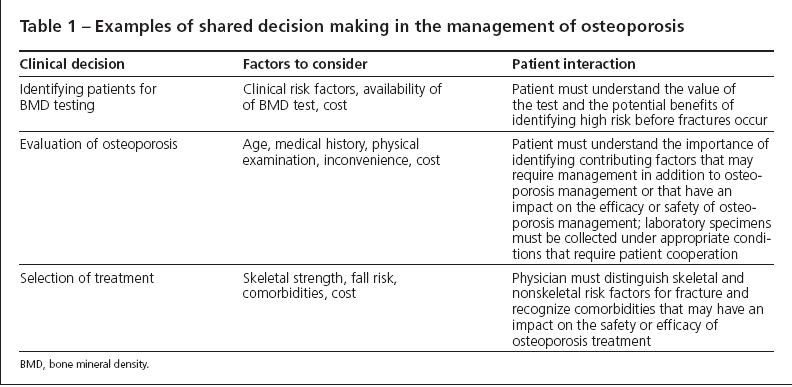
Several key clinical decisions are involved in osteoporosis management, including selection of patients for bone density testing, evaluation for factors contributing to low bone mass, identification of patients likely to benefit from treatment, recommendation of specific nonpharmacological and pharmacological therapies, and determination of how treatment is monitored. When physicians and their patients are educated about osteoporosis and have a full understanding of the risk and consequences of osteoporotic fractures, management decisions are most likely to result in successful clinical outcomes (Table 1). In this article, I address common clinical decision points in the form of responses to questions that often arise in the primary care practice setting.
COMMON QUESTIONSWho should have a bone density test?
The International Society for Clinical Densitometry (ISCD) has developed comprehensive guidelines for selecting patients to have a bone density test (Table 2).6 The organization also has created standards for acquisition, analysis, and interpretation of the test results.
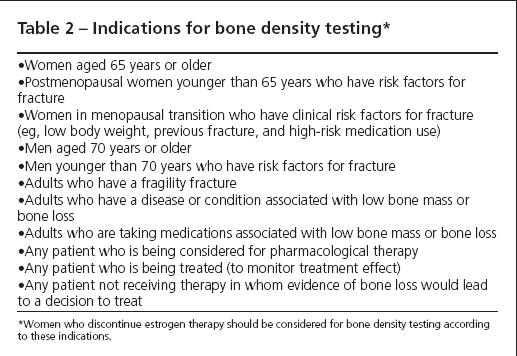
The ISCD Official Positions are an essential reference for bone densitometrists and a helpful guide for primary care physicians caring for patients who are at risk for osteoporosis. The unifying consideration is that a bone density test should be ordered only when it is likely to play a role in patient management decisions.
All women aged 65 years and older and men aged 70 years and older should be considered for bone density testing. Others who should be considered include women in menopausal transition and postmenopausal women younger than 65 years and men younger than 70 years who have risk factors for fracture (eg, a family history of osteoporosis, cigarette smoking, a personal history of fragility fracture, and taking a medication that is known to have adverse skeletal effects).
The only technology that can be used for diagnostic classification is dual-energy x-ray absorptiometry (DEXA). Technologies that can predict fracture risk include quantitative ultrasonography, quantitative computed tomography (QCT), peripheral QCT, and peripheral DEXA. Only DEXA and QCT are clinically useful for monitoring changes, provided that the precision error has been measured according to standard methods. T-score values measured by QCT are lower than T-scores measured by DEXA.
How is a diagnosis of osteoporosis established?
Assuming that other causes of skeletal fragility have been eliminated, 1 of 2 methods may be used. A densitometric diagnosis of osteoporosis is made according to the criteria of the World Health Organization (WHO) when a DEXA-measured T-score (the standard deviation [SD] difference between the patient’s BMD and that of a young-adult reference population) is −2.5 or lower at the hip (total hip, femoral neck); the posteroanterior lumbar spine (preferably L1-L4); or, if measured, the forearm (33% radius) (Table 3).7 The WHO diagnostic criteria may be applied to women in menopausal transition, postmenopausal women, and men aged 50 years and older.
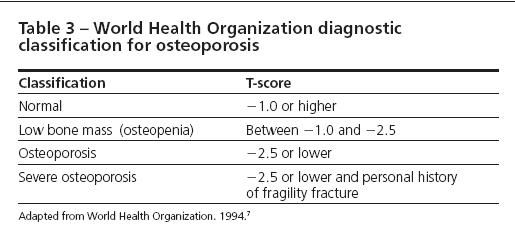
For younger women and men, the Z-score (the SD difference between the patient’s BMD and that of an age- and ethnicity-matched reference database) is preferred. The WHO classification should not be used, because the relationship between BMD and fracture risk is not well established in these groups. T-scores should not be used in children or adolescents, because comparing their BMD with that of an adult population that has already achieved peak bone mass would be inappropriate. A clinical diagnosis of osteoporosis may be made independently of the T-score by DEXA when there is a history of fragility fracture.
Diagnostic classification is useful for communicating disease-state information to the patient and may be needed for billing and determination of treatment benefits. A patient who is given a diagnosis of osteoporosis may gain a better understanding of its implications by observing the consequences (eg, fractures, disability, death) in others who have the same diagnosis. In the United States, a diagnosis code is required for payment for medical services and insurance coverage for treatment often requires a specific diagnosis.
How should patients who have low BMD be evaluated?
Baseline laboratory studies for all patients who have osteoporosis or low bone mass are useful for detecting previously unrecognized factors that may be contributing to poor skeletal health. They also may help determine the potential safety of specific drugs being considered for therapy.
There is no consensus guideline for standard laboratory evaluation, but there are helpful tests for all patients. These include serum calcium, phosphorus, and alkaline phosphatase levels (results may be abnormal in some types of metabolic bone disease, such as osteomalacia and malignancy); creatinine level (chronic kidney disease may result in skeletal disease and may affect the choice of drug therapy); complete blood cell count (may be abnormal with multiple myeloma or other malignant conditions); and 24-hour urinary calcium level (hypocalciuria in patients with adequate calcium intake and good renal function suggests malabsorption; hypercalciuria is associated with osteoporosis and an increased risk of nephrolithiasis).
The measurement of serum 25-hydroxyvitamin D often helps the evaluation because suboptimal levels are common. For optimal skeletal health, many experts recommend attaining a level of at least 30 ng/mL. In older patients, consider ordering serum protein electrophoresis to evaluate for multiple myeloma. Measuring thyroid-stimulating hormone helps identify patients who are taking an excessive dose of thyroid medication. For patients with hypercalcemia, further evaluation should include a measurement of serum parathyroid level. For unusual clinical situations, other laboratory tests or double tetracycline transiliac nondecalcified bone biopsy may provide useful information.
How is fracture risk assessed?
DEXA combined with clinical risk factors for fracture provides a better estimate of fracture risk than DEXA or clinical risk factors alone. Numerous clinical risk factors are associated with an increased risk of fracture8; those that have been best validated in large long-term observational studies are listed in Table 4.9
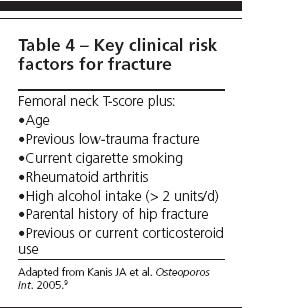
The most robust predictors of fracture are low BMD, advanced age, and previous fragility fracture. Fracture risk approximately doubles for every SD decrease in BMD and every decade advance in age, as well as in the presence of a fragility fracture. Fracture risk has been expressed as relative risk (the risk compared with that in a reference population, expressed as a ratio, such as “the relative risk of fracture is 2 times that of an age-matched population with normal BMD”). Now the field is moving rapidly toward expressing fracture risk as absolute risk (fracture probability over a defined period, such as “5% 10-year probability of hip fracture”). Fracture probability provides a better estimate of fracture risk for clinical applications, because relative risk may vary according to the comparator population that is selected.
Who should be treated?
Emerging methodologies will use fracture probability with country specific socioeconomic assumptions to estimate when treatment with pharmacological agents is likely to be cost-effective. This approach will provide more helpful information in the decision-making process than current guidelines, which usually recommend treatment based on T-score and clinical risk factors qualitatively rather than quantitatively.
The National Osteoporosis Foundation guidelines established in 2003 recommend treatment if the T-score is lower than −1.5 and clinical risk factors are present or if the T-score is lower than −2.0 regardless of clinical risk factors. These recommendations apply only to postmenopausal white women.
Updated guidelines (not yet released) are expected to use the WHO methodology with US-specific fracture prevalence data and economic assumptions to determine a fracture probability at which the treatment will be cost-effective. This approach will apply to postmenopausal women and men aged 50 years and older of all ethnicities, but it can be used only in untreated patients and is only one of many factors that should be used in making treatment decisions. Other considerations include the patient’s comorbidities, patient preferences, expected adherence to therapy, and affordability and availability of medications. In previously treated patients, fracture risk assessment and treatment decisions will be made as they are now.
How should patients be treated?
All patients, including those with normal BMD, should be counseled on the importance of regular physical activity, adequate intake of calcium and vitamin D, and avoidance of cigarette smoking and excess alcohol use. Care should be taken to minimize their exposure to medications known to be toxic to bones and those that may cause sedation, hypotension, or disequilibrium. Frail patients at high risk for falls may benefit from physical therapy or activities (eg, Tai Chi) that can improve muscle strength and balance. Impaired hearing or limited vision also may contribute to fall risk and, when possible, should be corrected. If fracture risk is sufficiently high, pharmacological therapy should be considered.
Oral bisphosphonates are the most frequently used drugs in the management of osteoporosis. Those approved by the FDA and available for clinical use are alendronate (10 mg/d or 70 mg/wk orally), risedronate (5 mg/d or 35 mg/wk orally), or ibandronate (150 mg/mo orally). All these agents increase BMD, reduce bone turnover, and decrease the risk of vertebral fractures.10 Alendronate and risedronate also have been shown to reduce the risk of nonvertebral fractures and hip fractures. These drugs must be ingested with a glass of plain water soon after awakening on an empty stomach after an overnight fast, followed by upright posture and postdose fasting (for at least 30 minutes with alendronate or risedronate and 60 minutes with ibandronate).
Two injectable bisphosphonates are FDA-approved for the management of postmenopausal osteoporosis-ibandronate (150 mg every 3 months, injected over 15 to 30 seconds) and zoledronic acid (5 mg every 12 months, injected over at least 15 minutes). Other FDA-approved pharmaceutical options are raloxifene (60 mg/d), a selective estrogen receptor modulator (SERM) that has been proved to reduce vertebral fracture risk and the risk of invasive breast cancer in high-risk women; salmon calcitonin (200 IU, intranasally, once daily); and teriparatide (20 µg/d by self-administered subcutaneous injection; maximum treatment period, 24 months), the only approved anabolic agent for the management of osteoporosis. These medications are listed with their indications in Table 5.
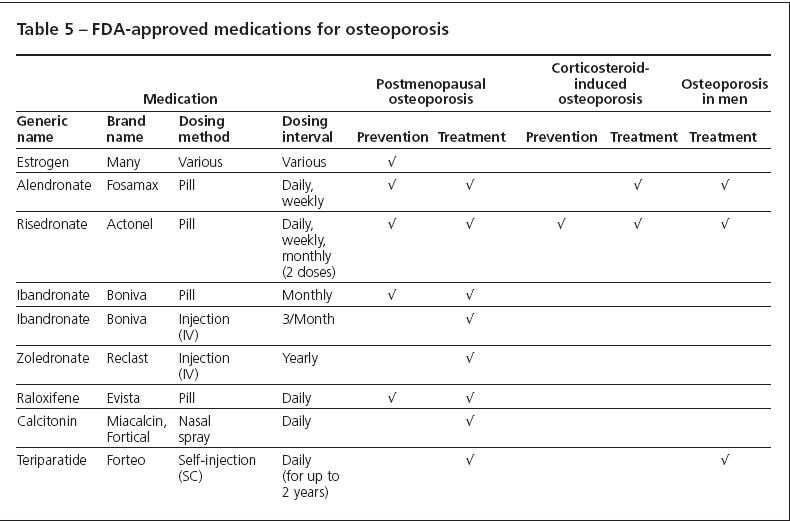
Each drug plays a role in osteoporosis prevention or treatment or both in properly selected patients, and each has its own profile of potential benefits and risks. The drugs cannot be ranked in terms of comparable efficacy, because no completed head-to-head clinical trials with fractures as a primary end point have been published. Ultimately, the best drug for a patient may be the one most likely to be taken, because poor compliance and persistence with therapy are major obstacles to achieving full drug benefits.5
An oral bisphosphonate usually is first-line therapy in appropriately selected patients. However, the recent availability of injectable bisphosphonates with long dosing intervals makes these agents attractive alternatives for patients who cannot take oral bisphosphonates and a possible consideration for primary therapy. Raloxifene most often is used in postmenopausal women younger than 65 years in whom the risk of thromboembolic and cardiovascular disease is not high and hot flashes are not a problem, especially those at high risk for breast cancer. Nasal calcitonin should be considered in women with osteoporosis who are at least 5 years postmenopausal and unable or unwilling to use other approved treatments. Teriparatide is reserved for use in patients at high risk for fracture and usually is followed by an antiresorptive drug, such as a bisphosphonate.
How should patients be monitored for response to therapy?
The response to therapy is commonly assessed by repeating DEXA of the spine and hip at least 1 year after the start of therapy. An acceptable response is considered to be stability or an increase in BMD, both of which have been associated with a reduction in fracture risk in clinical trials. Patients who have bone loss equal to or greater than the “least significant change,” calculated according to recognized standards,11 are candidates for a thorough evaluation to search for factors contributing to bone loss.12 A suboptimal response to therapy may be the result of poor compliance, inadequate calcium or vitamin D intake, malabsorption, bonetoxic medications, or the development of a previously unrecognized disease or conditions with adverse skeletal effects.
Measurement of bone turnover markers (eg, N- and C-telopeptide in patients taking antiresorptive therapy) may be used to evaluate drug effect on bone metabolism, which occurs sooner than changes in BMD.13 However, standards for their clinical use have not yet been established.
For how long should patients be treated?
The decision to start therapy is easier to make than the decision to stop therapy or suggest a “drug holiday.” There are no consensus guidelines on stopping therapy.
As a group, the bisphosphonates are known to have a long skeletal half-life; therefore, patients who have been taking bisphosphonates for several years probably will have some residual effects for an undefined period after discontinuation. Alendronate, the bisphosphonate that has been studied most extensively, appears to be safe and effective for as long as 10 years.14 Oversuppression of bone turnover, resulting in “brittle bones” with increased fracture risk or poor fracture healing, has been a theoretical concern since the introduction of the bisphosphonates. However, it does not seem to be a legitimate clinical concern.
The estrogens, SERMs, salmon calcitonin, and teriparatide may be expected to lose their benefits soon after discontinuation. Prudence suggests continuing treatment for as long as fracture risk is high, heeding FDA labeling that restricts teriparatide use to no more than 24 months until contradictory evidence becomes available, and considering no more than a 1-year holiday in patients who have taken alendronate for at least 5 years and are not currently at very high risk for fracture.15
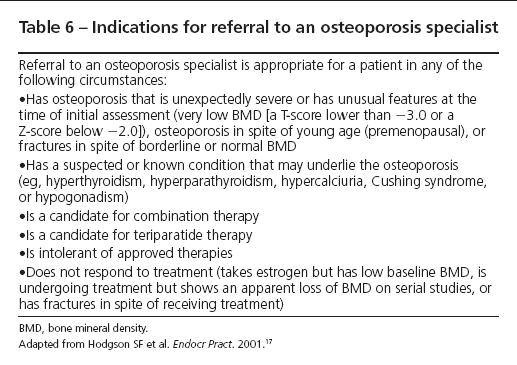
When should patients be referred to a specialist?
Most physicians are well qualified to manage the majority of patients with osteoporosis. However, referral to an osteoporosis specialist should be considered when the complexities of care exceed a physician’s comfort level. Common reasons for referral include significant BMD loss while the patient is receiving therapy, recurring fractures during therapy, fractures occurring with normal BMD, and unexplained skeletal-related laboratory test results. The American Association of Clinical Endocrinologists has identified specific indications for referral (Table 6).16
SUMMARY
Osteoporosis is associated with an increased risk of fractures and serious clinical consequences, but the condition often is underdiagnosed and undertreated. Physicians familiar with current strategies can manage most patients effectively. Patients educated about osteoporosis and actively involved in making decisions about their evaluation and treatment are most likely to adhere to therapy and benefit from a reduced risk of fractures.
References:
References
- 1. Klibanski A, Adams-Campbell L, Bassford T, etal. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285:785-795.
- 2. van Staa TP, Dennison EM, Leufkens HG, Cooper C. Epidemiology of fractures in England and Wales. Bone. 2001;29:517-522.
- 3. Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465-475.
- 4. Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med. 1997;103(2A):12S-19S.
- 5. Cramer JA, Gold DT, Silverman SL, Lewiecki EM. A systematic review of persistence and compliance with bisphosphonates for osteoporosis. Osteoporos Int. 2007;18:1023-1031.
- 6. Binkley N, Bilezikian JP, Kendler DL, et al. Official positions of the International Society for Clinical Densitometry and Executive Summary of the 2005 Position Development Conference. J Clin Densitom. 2006;9:4-14.
- 7. World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Geneva: WHO;1994.
- 8. Physician’s Guide to Prevention and Treatment of Osteoporosis. Washington, DC: National Osteoporosis Foundation; 2003.
- 9. Kanis JA, Borgstrom F, De Laet C, et al. Assessment of fracture risk. Osteoporos Int. 2005;16:581-589.
- 10. Cranney A, Guyatt G, Griffith L, et al. Meta-analyses of therapies for postmenopausal osteoporosis, IX: summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev. 2002;23:570-578.
- 11. Lenchik L, Kiebzak GM, Blunt BA, International Society for Clinical Densitometry Position Development Panel and Scientific Advisory Committee. What is the role of serial bone mineral density measurements in patient management? J Clin Densitom. 2002;5(suppl):S29-S38.
- 12. Lewiecki EM. Nonresponders to osteoporosis therapy. J Clin Densitom. 2003;6:307-314.
- 13. Srivastava AK, Vliet EL, Lewiecki EM, et al. Clinical use of serum and urine bone markers in the management of osteoporosis. Curr Med Res Opin. 2005;21:1015-1026.
- 14. Bone HG, Hosking D, Devogelaer JP, et al. Ten years’ experience with alendronate for osteoporosisin postmenopausal women. N Engl J Med. 2004;350:1189-1199.
- 15. Black DM, Schwartz AV, Ensrud KE, et al. Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA. 2006;296:2927-2938.
- 16. Hodgson SF, Watts NB, Bilezikian JP, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the prevention and treatment of postmenopausal osteoporosis: 2001 edition, with selected updates for 2003 [published correction appears in Endocr Pract. 2004;10:90]. Endocr Pract. 2003;9:544-564.
- 17. Hodgson SF, Watts NB, Bilezikian JP, et al. American Association of Clinical Endocrinologists 2001 Medical Guidelines for Clinical Practice for the Prevention and Management of Postmenopausal Osteoporosis. Endocr Pract. 2001;7:293-312.