Managing Hip Fractures in Older Patients: Perioperative Decision Making
ABSTRACT: Hip fractures in older patients are projected to increase infrequency as the US population continues to age.
ABSTRACT: Hip fractures in older patients are projected to increase in frequency as the US population continues to age. A thorough history and physical examination is essential. The initial workup should include radiographic imaging. Operative stabilization is the treatment of choice for most femoral neck or intertrochanteric hip fractures. The goals should be to achieve a stable reduction to allow for early patient mobilization, restore the patient's preinjury level of function, and minimize the risk of medical complications. Postoperative complications are associated with mortality and diminished return of function. All patients with hip fractures should receive perioperative deep venous thrombosis chemoprophylaxis, unless it is contraindicated. A multidisciplinary approach to postoperative rehabilitation can shorten the inpatient stay and decrease the mortality rate. (J Musculoskel Med. 2008;25:326-336)
Hip fractures in older patients are associated with significant morbidity and mortality. They occur most frequently in these patients and are projected to increase in frequency as the US population continues to age.
A thorough history and physical examination is essential to ensure that medical management of comorbidities before surgical intervention is optimized and to evaluate other potential injuries associated with the inciting event. The patient's functional and social status should be assessed to help predict and plan the clinical outcome. Each patient's functional goals are critical factors in surgical decision making; these goals should be considered by the patient, his or her family, the primary care physician, and the surgeon. In determining the ideal setting for reaching rehabilitation goals, coordination between a social worker, case manager, physiatrist, and the patient and his family is invaluable.
In older patients, we perform operative fixation with screws in nondisplaced fractures and either hemiarthroplasty or total hip arthroplasty in displaced fractures; in younger patients, we attempt closed or open reduction and operative fixation in almost all fractures. We avoid use of a hemiarthroplasty or total hip arthroplasty in younger patients because they probably will outlast the life span of the implant and subsequently require revision surgery (or surgeries). The younger and more active the patient, the more likely (and earlier) he will wear out his prosthesis and require a revision,which will result in less bone stock with each subsequent surgery. Therefore, we attempt operative fixation after reduction in almost all younger patients.
In this article, we describe the epidemiology of hip fractures in older patients, the medical evaluation, and the surgical options and risk factors. We also discuss the postoperative complications and rehabilitation.
EPIDEMIOLOGY
About 250,000 hip fractures occur in the United States each year at an annual cost of about $9 billion.1 Based on conservative assumptions, the population of US persons 65 years and older is projected to grow to 78 million in the year 2050 from 35 million in 20001; accordingly, the incidence of hip fractures is expected to double by 2050.2
Trochanteric hip fractures represent almost half of proximal femur fractures; the female-to-male ratio ranges from 2:1 to 8:1.3 The average patient age at which trochanteric hip fractures occur is 82.1 years; for femoral neck fractures, the average age is 77.9 years.4 Women have 80% of trochanteric hip fractures; the incidence doubles for each decade after age 50 years.
The mortality rates of femoral neck and intertrochanteric fractures are comparable, ranging from 14% to 50% within the first year after injury. The highest mortality occurs within the first 4 to 6 months after fracture. Mortality rates are higher in men and patients older than 75 years than in women and younger persons.5 However, Aharonoff and coworkers6 showed a 1-year mortality rate of only 12.7% for older patients with a hip fracture who were community dwelling and cognitively intact.
MEDICAL EVALUATION
The patient's initial workup should include radiographic imaging of any painful or ecchymotic areas of the body. A complete blood cell count,coagulation profile, and electrolyte panel should be obtained because many older patients live alone and may experience long delays before treatment, resulting in dehydration and poor nutrition. A Foley catheter should be used to monitor urinary output adequately and help hemodynamic monitoring.
Osteoporosis often results in "insufficiency" fractures-fractures that occur in compromised or weakened bone after a physiologic load. Hip fractures tend to occur after a traumatic episode.Although osteoporosis may be a confounding factor, trauma usually is the cause.
In some older patients, cardiopulmonary disease is a major factor that may affect the ability to tolerate surgery and rehabilitation; obtaining an internal medicine consultation on admission for preoperative medical optimization is desirable. In addition, chemoprophylaxis and/or mechanical prophylaxis against deep venous thrombosis (DVT) should be instituted as early as possible because patients may be immobile for up to 2 days. If low-molecular-weight heparin is administered, it should be discontinued 12 to 24 hours before surgery.
SURGERY
Timing
Operative stabilization is the treatment of choice for a patient with nearly any femoral neck or intertrochanteric hip fracture. Nonoperative management of hip fractures in older patients is associated with extremely high mortality rates and limited functional recovery; therefore, such an approach should be reserved for those "too sick" to undergo repair.
With all hip fracture surgery, the goals are to achieve a stable reduction to allow for early patient mobilization, restore the patient's preinjury level of function, and minimize the risk of medical complications. Toward these ends, early treatment with surgical stabilization is recommended.
When operative treatment is indicated, proceeding with surgery as soon as the patient's condition has been medically optimized and cleared for surgery is best. Zuckerman and associates7 prospectively studied 367 patients who had a hip fracture to determine the effect of an operative delay on postoperative complications and on the 1-year mortality rate.When the patients' age, sex, and number of medical comorbidities were controlled, an operative delay beyond 3 days doubled the mortality rate by the end of the first postoperative year.
Anesthetic
Choice of anesthetic technique has not been proved to have an impact on the mortality rate in older patients with hip fractures. Bigler and colleagues8 compared the effect of general anesthetic with that of spinal anesthetic on mental function and morbidity up to 3 months postoperatively in 40 older patients (mean age, 78.9 years) undergoing acute hip fracture surgery. The authors noted no persistent mental impairment in either group, and there was no difference in mortality or complication rate. However, there was a shorter time to ambulation in those who received spinal anesthetic.
In a case series of 631 community-dwelling older patients who sustained a femoral neck or intertrochanteric hip fracture, patients were evaluated prospectively to determine the effect, if any, of anesthetic technique on ambulatory ability and percent functional recovery at 3, 6, and 12 months after hip fracture.9 The authors noted a significant increase in recovery of ambulatory ability and percent functional recovery at 6 months in patients who had received general anesthetic. After controlling for potential confounding variables,however, they observed no differences between groups at any of the time intervals.
Surgical implants
Surgeons must understand the implant options available and try to achieve accurate alignment and proper implant positioning. Surgical options for femoral neck fractures include internal fixation with cannulated screws and replacement-either a hemiarthroplasty (replacing the femoral head and neck) or a total hip arthroplasty, which includes the femoral head, neck, and acetabulum.The decision to repair or replace is based on a variety of factors, including the fracture pattern, the patient's functional status, medical comorbidities and, if present, preoperative hip symptoms.
For nondisplaced or minimally displaced femoral neck fractures, the use of 3 cannulated screws-via an open or closed approach (Figures 1 and 2)-has proved to be the gold standard. The treatment of choice for displaced femoral neck fractures in older patients is a hemiarthroplasty (Figures 3 and 4) or total hip arthroplasty; a variety of implants are available, depending on the surgeon's preference.When implant options for arthroplasty are being considered, the choice of manufacturer is less important than the choice of implant type (eg, hemiarthroplasty vs total hip arthroplasty).
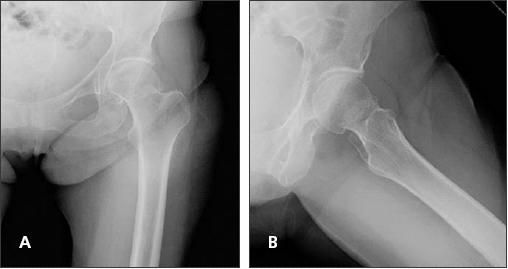
Figure 1
–
Anteroposterior (A) and lateral (B) radiographs of an 83-year-old woman obtained after a mechanical trip and fall demonstrate a valgus-impacted left femoral neck fracture.

Figure 2 –
Percutaneous pinning of the left femoral neck fracture is seen in anteroposterior pelvis (A) and lateral (B) radiographs obtained 6 weeks post closed reduction.
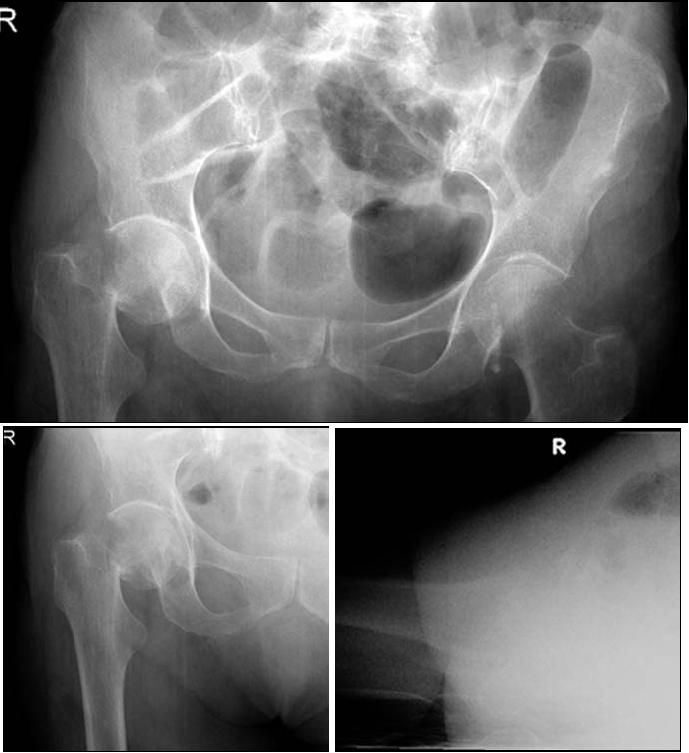
Figure 3 –
Anteroposterior (A), traction and internal rotation (B), and lateral (C) radiographs of an 83-year-old woman obtained after a mechanical trip and fall demonstrate a displaced right femoral neck fracture.
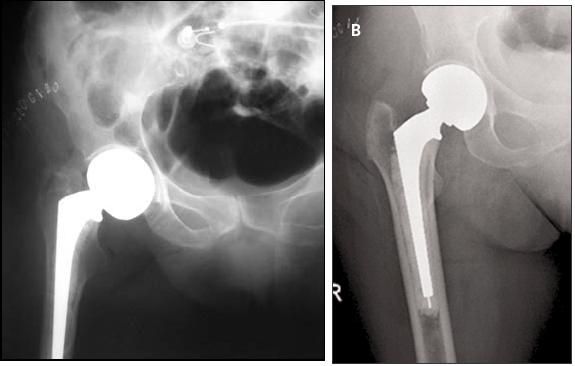
Figure 4 –
Anteroposterior pelvis (A) and right hip (B) radiographs post right hip hemiarthroplasty are shown here.
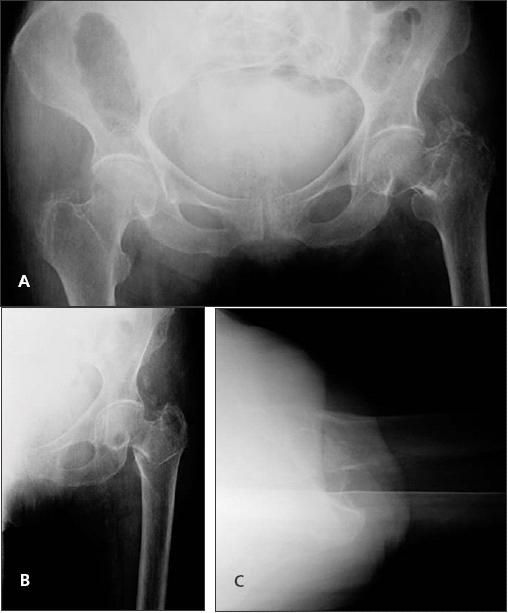
Figure 5 –
Anteroposterior pelvis (A), traction and internal rotation (B), and lateral (C) radiographs of an 89-year-old woman obtained after a mechanical trip and fall demonstrate a left intertrochanteric hip fracture.
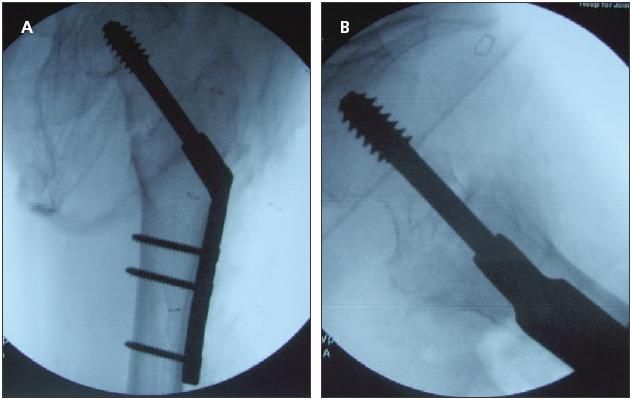
Figure 6 –
Shown are anteroposterior (A) and lateral (B) views of the left hip post placement of a dynamic hip-screw of a left hip intertrochanteric fracture.
The most frequently used devices for surgical management of intertrochanteric fractures are the compression hip-screw with a sideplate (Figures 5 and 6) and a cephalomedullary nail device. Although the compression hip-screw traditionally has been the gold standard, numerous clinical studies have cited equal efficacy of the devices when morbidity, mortality, and wound complications were compared.
Hardy and colleagues10 reviewed the results of 100 older patients with an intertrochanteric femoral fracture randomized to treatment with a compression hip-screw with a plate or an intramedullary hipscrew. They concluded that results obtained with the newer intramedullary devices correlate with the experience and comfort level of the surgeon. However, it has been well-documented that based on the biomechanical construct of cephalomedullary nails, more complex intertrochanteric fractures with subtrochanteric extension or reverse obliquity patterns are better suited for intramedullary nail fixation, rather than with a compression hip-screw.
Risk factors and return to preinjury function
Risk factors for patient mortality and return to preinjury functional status have been looked at extensively. In a prospective study of 537 patients who had hip fracture and at least 6 months of follow-up, only patient age and preinjury functional independence measure scores were independent predictors of functional outcome.11
Koval and colleagues12 prospectively reviewed 336 community dwelling, previously ambulatory geriatric patients with hip fractures to determine ambulatory ability at a minimum follow-up of 1 year. In this series, 40.8% of patients maintained their prefracture ambulatory ability, 39.9% remained ambulatory but became more dependent on assistive devices, 11.6% previously were community ambulators and became household ambulators, and 7.7% became nonfunctional ambulators. The authors identified patient age, prefracture ambulatory ability, American Society of Anesthesiologists rating of operative risk, and fracture type as significant predictors of ambulatory recovery.
POSTOPERATIVE COMPLICATIONS
Postoperative complications are associated with mortality and diminished return of function. Therefore, the treating medical and surgical teams need to prevent complications. Toward this end, a primary goal of treatment of any older patient who has sustained a hip fracture is immediate mobilization. This serves to minimize the morbidities associated with prolonged recumbency, including pulmonary complications, decubitus ulcers, and muscle atrophy.
Restrict weight bearing?
All patients who undergo internal fixation should be allowed to bear weight as tolerated; restricted weight bearing may delay the patient's functional recovery and return to independent living. In 1984, Arnold13 studied 199 femoral neck fractures in 197 patients who were treated with Knowles pins and allowed early weight bearing (before radiographic evidence of healing); his results were comparable with those of a similar group of patients with femoral neck fractures who were non–weight bearing. He concluded that as long as the fractures are properly reduced and pinned, early weight bearing does not adversely affect the stability of a femoral neck fracture.
Koval and associates14 prospectively evaluated the results of 596 geriatric patients who sustained femoral neck or intertrochanteric fractures and had a minimum of 1 year of follow-up. All patients were permitted immediate unrestricted weight bearing; 16 patients required additional hip surgery. Of the 473 patients available for follow-up, 138 had stable and 70 had unstable intertrochanteric fractures. Six patients required revision surgery; all had loss of fixation because of lag screw cutout of the femoral head and neck, and 5 revisions could be attributed to poor surgical technique. The revision rate was 5.3% after internal fixation of the femoral neck from loss of fixation/nonunion, 5.4% from osteonecrosis for patients with 2-year follow-up, and 0.6% after hemiarthroplasty because of prosthetic dislocation.The results compare favorably with reports of restricted weight bearing and support the use of unrestricted weight bearing in older patients after hip fracture surgery.
In another study, Koval and colleagues15 evaluated older patients who were allowed to bear weight as tolerated after operative treatment of femoral neck or intertrochanteric hip fractures; they used computerized gait testing to quantify weight bearing. The results demonstrated that patients without evidence of dementia limit their own weight bearing of the injured limb as they progress in the postoperative period. During the first 3 weeks, the patients who had had internal fixation bore substantially less weight than those who had had a hemiarthroplasty. By 6 weeks, there were no significant differences in weight bearing in the groups. In addition, patients with unstable fractures were found to self-limit their weight bearing more than those with stable fracture patterns. The results further emphasize the rationale for making older patients weight-bearing as tolerated after operative fixation of hip fractures and that restricting weight bearing can delay functional recovery.
Infection and venous thromboembolism prophylaxis
Perioperative administration of a first-generation cephalosporin for 24 hours has been shown to decrease the incidence of postoperative infections.16 Clindamycin or vancomycin may be substituted in patients who have serious adverse reactions to β-lactam antibiotics. Prophylactic use of antibiotics beyond 24 hours postoperatively until all catheters and drains are removed has not been proved to lower infection rates.17
Although the ideal regimen for DVT prophylaxis is controversial, it is widely accepted that all patients with hip fracture should receive perioperative chemoprophylaxis. The American College of Chest Physicians currently recommends low-molecular-weight heparin, low-dose unfractionated heparin, fondaparinux, or warfarin for DVT prophylaxis in these patients.18 In the recovery room after surgery, intermittent pneumatic impulse boots or sequential compression devices are placed on both of the patient's lower extremities, unless there is suspicion of DVT. In addition, incentive spirometry and deep breathing exercises are instituted and the patient is encouraged to perform them on an hourly basis when awake throughout the remainder of the hospital course.
POSTOPERATIVE REHABILITATION
Physical therapy and occupational therapy
These should be initiated on postoperative day one, beginning with mobilization from the bed to the chair. If the patient cannot tolerate this transfer, he is assisted into the dangling position. In physical therapy, strengthening exercises should progress with each session, beginning with active-assisted exercises and progressing to active exercises until resistance exercises are completed. Each person should have a therapy program tailored to his preoperative level of function and physical, psychological, and social circumstances.
Occupational therapy should focus on helping persons regain coordination and perceptual, motor, and adaptive skills to achieve independence in their activities of daily living (ADLs) (eg, toileting, dressing, bathing, and cooking). In our experience, most older patients who sustain a femoral neck or intertrochanteric fracture benefit from a course of inpatient rehabilitation; therefore,we obtain a rehabilitation consultation on the first postoperative day for disposition planning.
Multidisciplinary approach
The patient's rehabilitation goals and disposition should be reevaluated daily. For those who wish to be discharged home from the acute orthopedic service, the appropriate arrangements should be made for outpatient physical and occupational therapy once the patient is deemed ready for discharge.
Despite advances in surgical fixation techniques, hip fractures still impose a physical, psychological, and financial burden on the patient, as well as family and caregivers. In addition, outcomes for older patients who sustain a hip fracture often fall short of expectations, even with improvements in implant technology, operative technique, and rehabilitation protocols. The ability to regain a prefracture level of function and independence may not be realized even if the surgical management (fracture healing or prosthetic replacement) has been successful.19
Therefore, the physician needs knowledge of both positive and negative predictors of functional outcome to identify at-risk patients so that modifications of the treatment approach, discharge planning, and use of health care resources can be implemented. For example, patients with an intertrochanteric hip fracture who were anemic on presentation to the hospital were found to have an increased length of hospital stay, as well as higher mortality rates at 6 and 12 months.20
In addition, patients who had an abnormal albumin level and total lymphocyte count were 2.9 times more likely to have a length of stay greater than 2 weeks and 3.9 times more likely to die within 1 year after surgery. They also were 4.6 times less likely to recover their prefracture level of independence in basic ADLs.21
The literature over the past 5 years has proved that dedicated diagnostic and treatment algorithms for older patients with hip fractures can both shorten the acute inpatient stay and improve treatment outcomes.2 A multidisciplinary approach that involves orthopedists, internists, physiatrists, social workers, and therapists can serve to shorten the inpatient stay and decrease the acute and 1-year mortality rate.
Primary care physician involvement is crucial in this patient population. The primary care physician knows the patient's baseline medical (physical function and mental) status. In addition to providing optimal medical preparation of the patient for surgery, the primary care physician will be managing his medical comorbidities during the postoperative course and after discharge.
References:
References
1.
Shabat S. Hip fractures in elderly patients-perspectives towards the future.
Disabil Rehabil.
2005;27:1039-1040.
2.
Koval KJ, Chen AL, Aharonoff GB, et al. Clinical pathway for hip fractures in the elderly: the Hospital for Joint Diseases experience.
Clin Orthop Relat Res.
2004;425:72-81.
3.
Koval KJ, Zuckerman JD. Hip fractures, II: evaluation and treatment of intertrochanteric fractures.
J Am Acad Orthop Surg.
1994;2:150-156.
4.
Court-Brown C, Koval K. Epidemiology. In: Bucholz RW, Heckman JD, Court-Brown C, et al, eds.
Rockwood and Green’s Fractures in Adults.
6th ed. Vol 1. Philadelphia: Lippincott Williams & Wilkins; 2006:110.
5.
Koval KJ, Cooley MR. Clinical pathway after hip fracture.
Disabil Rehabil.
2005;27:1053-1060.
6.
Aharonoff GB, Koval KJ, Shovron ML, Zuckerman JD. Hip fractures in the elderly: predictors of one year mortality.
J Orthop Trauma.
1997;11:162-165.
7.
Zuckerman JD, Shovron ML, Koval KJ, et al. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip.
J Bone Joint Surg.
1995;77A:1551-1556.
8.
Bigler D, Adelhoj B, Petring OU, et al. Mental function and morbidity after acute hip surgery during spinal and general anaesthesia.
Anaesthesia.
1985;40:672-676.
9.
Koval KJ, Aharonoff GB, Rosenberg AD, et al. Functional outcome after hip fracture: effect of general versus regional anesthesia.
Clin Orthop Relat Res.
1998;348:37-41.
10.
Hardy DC, Descamps PY, Krallis P, et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures: a prospective, randomized study of one hundred patients.
J Bone Joint Surg.
1998;80A:618-630.
11.
Cornwall R, Gilbert MS, Koval KJ, et al. Functional outcomes and mortality vary among different types of hip fractures: a function of patient characteristics.
Clin Orthop Relat Res.
2004;425:64-71.
12.
Koval KJ, Skovron ML, Aharonoff GB, et al. Ambulatory ability after hip fracture: a prospective study in geriatric patients.
Clin Orthop Relat Res.
1995;310:150-159.
13.
Arnold WD. The effect of early weight-bearing on the stability of femoral neck fractures treated with Knowles pins.
J Bone Joint Surg.
1984;66A:847-852.
14.
Koval KJ, Friend KD, Aharonoff GB, Zuckerman JD. Weight bearing after hip fracture: a prospective series of 596 geriatric hip fracture patients.
J Orthop Trauma.
1996;10:526-530.
15.
Koval KJ, Sala DA, Kummer FJ, Zuckerman JD. Postoperative weight-bearing after a fracture of the femoral neck or an intertrochanteric fracture.
J Bone Joint Surg.
1998;80A:352-356.
16.
Burnett JW, Gustilo RB, Williams DN, Kind AC. Prophylactic antibiotics in hip fractures: a double-blind, prospective study. J Bone Joint Surg. 1980;62A:457-462.
17.
Bratzler DW, Houck PM; Surgical Infection Prevention Guidelines Writers Workgroup, et al. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project.
Clin Infect Dis.
2004;38:1706-1715.
18.
Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy.
Chest.
2004;126(3 suppl):S338-S400.
19.
Egol KA, Koval KJ, Zuckerman JD. Functional recovery following hip fracture in the elderly.
J Orthop Trauma.
1997;11:594-599.
20.
Gruson KI, Aharonoff GB, Egol KA, et al. The relationship between admission hemoglobin level and outcome after hip fracture.
J Orthop Trauma.
2002;16:39-44.
21.
Koval KJ, Maurer SG, Su ET, et al. The effects of nutritional status on outcome after hip fracture.
J Orthop Trauma.
1999;13:164-169.
Â