Q&A: Guselkumab in Active Psoriatic Arthritis
In patients with psoriatic arthritis (PsA), guselkumab (Tremfya, Janssen Immunology) treatment reduced serum protein levels of acute phase and T-helper cell 17 (Th17) effector cytokines, achieving comparable levels to those in healthy controls.
In patients with psoriatic arthritis (PsA), guselkumab (Tremfya, Janssen Immunology) treatment reduced serum protein levels of acute phase and T-helper cell 17 (Th17) effector cytokines, achieving comparable levels to those in healthy controls, according to study data published in RMD Open1. Researchersalso showed thatreductions of interleukin (IL)-17A and IL-17F were greater after treatment with guselkumab than with ustekinumab (Stelara, Janssen Immunology).
In this Q&A, corresponding author Kristen Sweet, PhD, associate director of clinical research in rheumatology at Janssen Research & Development, Pennsylvania, discussed the research and its findings.
In the DISCOVER-1 and DISCOVER-2 studies, participants with PsA were treated with guselkumab or placebo. Serum levels of acute phase reactants C reactive protein (CRP) and serum amyloid A and inflammatory cytokines/chemokines were measured at baseline and at weeks 4 and 24 in 300 participants and in 34 healthy controls. The PSUMMIT studies measured serum IL-17A, IL-17F, and CRP after ustekinumab treatment and the results were compared with those reported after guselkumab treatment.
Rheumatology Network: Why was the trial conducted?
Kristen Sweet, PhD:DISCOVER-1 and DISCOVER-2 were phase 3 trials conducted to evaluate the efficacy and safety of the selective IL-23 inhibitor therapy, guselkumab, in patients with active PsA.
Serum samples were collected in DISCOVER-1 and DISCOVER-2 as an opportunity to better understand the biology of PsA, provide a biological assessment of the response of participants to treatment with guselkumab, analyze differences in biomarkers between clinical responders and non-responders, determine if these biomarkers can be used to classify participants as potential responders prior to treatment, and determine how inhibition of IL-23p19 versus IL-12/IL-23 differentially modifies cytokine expression.
RN: What were the surprises from the findings?
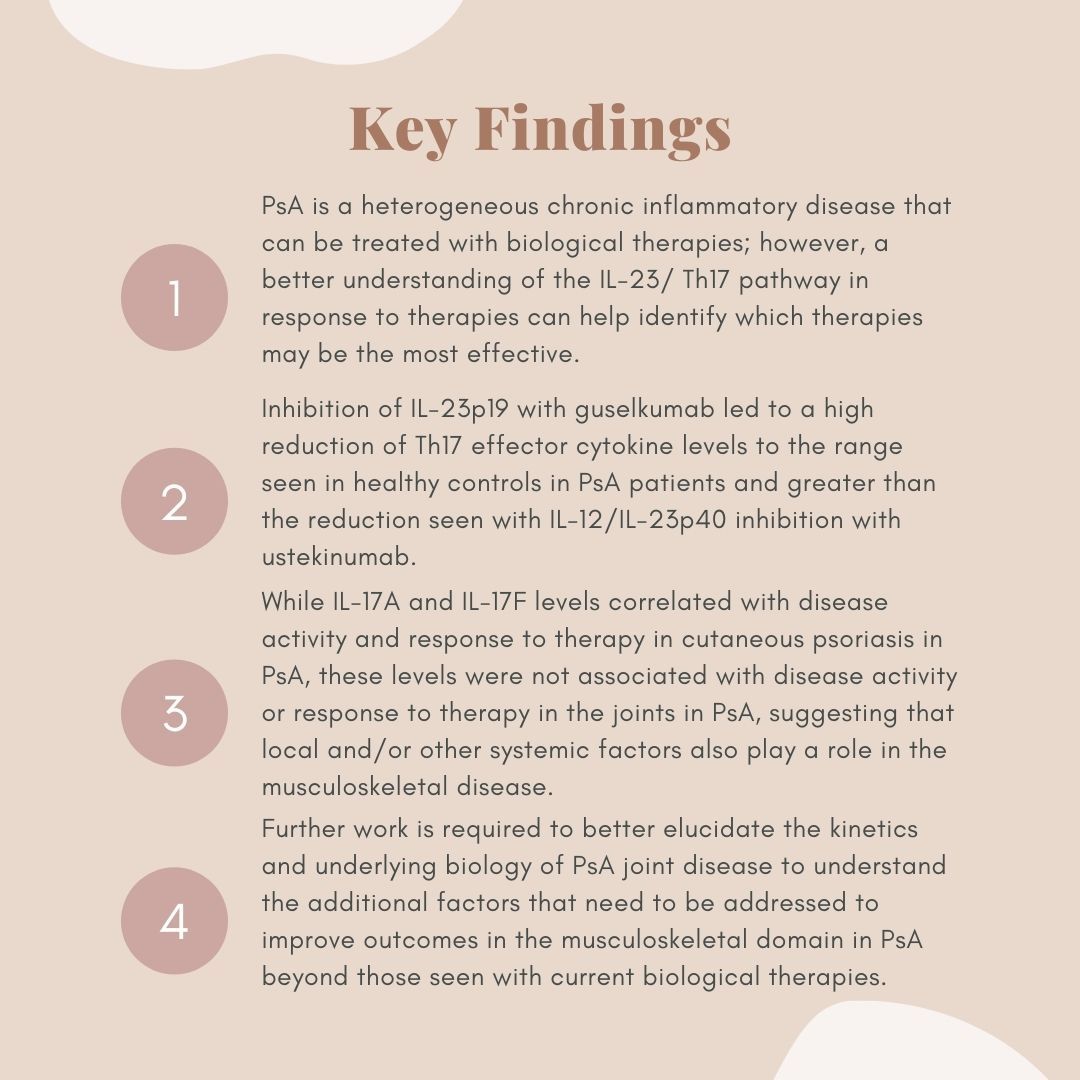
KS: Notably, inhibition of IL-23p19 with guselkumab led to a high reduction of Th17 effector cytokine levels to the range seen in healthy controls and greater than the reduction seen with IL-12/IL-23p40 inhibition with ustekinumab.
While IL-17A and IL-17F levels correlated with disease activity and response to therapy in cutaneous psoriasis in PsA, these levels were not associated with disease activity or response to therapy in the joints in PsA, suggesting that local and/or other systemic factors also play a role in the musculoskeletal disease.
RN: How significant are the results?
KS: This work is important as it furthers our understanding of the IL-23/Th17 pathway in response to therapies. The residual joint disease in the face of apparent “normalization” of serum IL-17A and IL-17F levels with guselkumab treatment indicates that further work is required to better elucidate the kinetics and underlying biology of PsA joint disease.
RN: What is the current practice and how could the findings possibly change things?
KS: In current clinical practice, treatment of PsA remains largely empirical, with many patients exhibiting no or only partial response to available therapies while others exhibit discordant responses in the skin and musculoskeletal system. As we advance understanding of how the IL-23/Th17 pathway responds to therapies, additional factors that need to be addressed can be investigated to improve outcomes in the musculoskeletal domain in PsA beyond those seen with current biologic therapies.
RN: What are the key takeaway points for clinicians who may be reading this article?
KS: The key takeaways for clinicians are:
Reference:
Sweet K, Song Q, Loza MJ, et al. Guselkumab induces robust reduction in acute phase proteins and type 17 effector cytokines in active psoriatic arthritis: results from phase 3 trials.RMD Open 2021;7:e001679. doi: 10.1136/rmdopen-2021-001679